Pan-European Networks of communities of people living with and affected by HIV, doctors and scientists call upon the Government of the Czech Republic to immediately stop the Prague Public Health Authority’s persecution and intimidation of people living with HIV, and to return to evidence-based and proven practices in HIV prevention, testing and care in the Czech Republic.
Brussels, 19 February 2016 – The signatories of this open letter, representing communities of people living with, and affected by HIV, doctors and scientists addressing HIV and co-infections in Europe, are extremely concerned that the Prague Public Health Authority has initiated a police investigation into the sex lives of 30 men living with HIV on the sole grounds that these men have been diagnosed with a sexually transmitted infection (STI).
We understand that the Czech police are currently conducting investigations and are considering pressing charges against these men claiming that they have violated the provisions of Sections 152 and 153 of the Czech Criminal Code.
There is no evidence that punitive approaches to regulating the consensual sexual behaviour of people with living HIV are an effective HIV prevention or public health tool, but there is evidence that such approaches can be counterproductive by further stigmatising people with HIV, sending those in need of testing and treatment underground, harming individual and public health.
In addition, the release of medical information to the police appears to be a grave violation of personal freedoms of individuals living in the Czech Republic. The initiation of criminal prosecution against people living with HIV for alleged intentional gross bodily harm – despite the lack of a single complainant – raises grave concerns regarding the inappropriate application of criminal law to people living with HIV.
We also understand that a number of non-governmental organizations have recently spoken out against the acts of the Prague Public Health Authority and subsequent police investigation and they will approach the Czech liaison at the UN High Commissioner for Human Rights. Please also note that the responsible UNAIDS representative has already been informed and will receive further briefing from us.
With this letter we express our outrage at these human rights violations, and support the groups within the Czech Republic who initially raised objections and are working to support both people with HIV and the public health of all those living in the country.
Our main objections to the recent development are based on several arguments:
- It violates the fundamental human right to personal integrity and privacy (Art 7 Sec. 1 of the Charter of Fundamental Rights and Freedoms), and breaches the Czech Republic’s international obligations under the existing National HIV/AIDS Strategy;
- It is counterproductive to public health, ignoring well established WHO and UNAIDS recommendations on appropriate use of public health and criminal law as it relates to HIV. Evidence shows that criminalisation of HIV non-disclosure, potential or perceived exposure or non-intentional transmission deter people from getting tested and force them to hide their HIV status and/or sexual orientation, thus reducing opportunities for treatment which greatly reduces infectiousness.
- There is a substantial body of evidence to show that the overly broad HIV criminalisation, in any form, is harmful for both individuals and society as it leads to increased latency of the epidemic, deters people from getting tested and treated, and thus ultimately contributes to a growing epidemic. We recognize that there has been a constant and alarming increase in the rate of new HIV infections in Europe in the last ten years. However, the active discrimination and violation of the human rights of any group of society will not contribute to the curbing of the epidemic.
- The proposed prosecution of people living with HIV for alleged intentional spread of infectious diseases, or in fact the transfer of any health-related data of individual from the health care system to law enforcement organisations is potentially a violation of the European Union’s Data Protection Directive.
We demand that the Government of the Czech Republic adheres to the international principles and treaties, and scientific evidence universally accepted in the practice of HIV prevention, and we also demand that the current level of HIV care in the country is maintained and improved to assure at-risk groups feel that getting tested for HIV is and should be a reasonable decision for them. Nothing is as effective in linking to and retention in care than disseminating the right information, and fighting stigma and discrimination against people living with HIV, or any other groups such as men having sex with men. The active discrimination and legal persecution of people with HIV is in diametrical opposition to this evidence.
The signatories will continue to support local non-governmental organisations and other actors in their efforts to prevent HIV criminalization becoming a public health policy. We call on the Government of Czech Republic to ensure that the Prague Public Health Authority reverses this policy and ends police investigations of people with HIV simply for being diagnosed with an STI and instead relies on good public health practice as the most effective strategy to deal with HIV/AIDS.
Speaking on behalf of millions of people living with and affected by HIV across Europe, as well as experts in HIV science, public health and human rights, the signatories are ready to provide advice, guidance and the collection of good practices relating to HIV prevention to the government.
Contact:
HIV Justice Network: Edwin J Bernard, edwin@hivjustice.net
European AIDS Treatment Group: Tamás Bereczky on tamas.bereczky@eatg.org
Download and share the letter (with references). Also available on the EATG website
Open Letter to Prague Public Health Authority
Footnote: At the request of Czech AIDS Society a number of organisations representing European networks of communities of people living with and affected by HIV, doctors and scientists wrote today to head of Prague’s Public Health Authority to raise our concern about the initiation of a police investigation into the sex lives of 30 men living with HIV on the sole grounds that these men have been diagnosed with a sexually transmitted infection (STI).
We hereby would like to stress that disseminating the right information, and fighting stigma and discrimination against people living with HIV, or any other groups such as men having sex with men has proved have proved to be effective in responding to the epidemic, to link to and retain persons in care. The active discrimination and legal persecution of people with HIV is in diametrical opposition to this evidence.
Letter to Dr. Zdeňka Jágrová, Hygienicka, Head of the Prague Public Health Authority
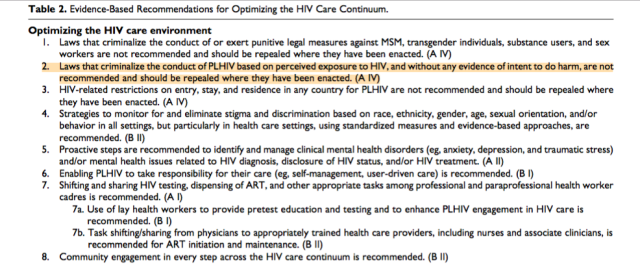 In many settings, optimizing the HIV care environment may be the most important action to ensure that there are meaningful increases in the number of people who are tested for HIV, linked to care, started on ART if diagnosed to be HIV positive, and assisted to achieve and maintain long-term viral suppression. Overcoming the legal, social, environmental, and structural barriers that limit access to the full range of services across the HIV care continuum requires multistakeholder engagement, diversified and inclusive strategies, and innovative approaches. Addressing laws that criminalize the conduct of key populations and supporting interventions that reduce HIV-related stigma and discrimination are also critically important. People living with HIV also require support through peer counseling, education, and navigation mechanisms, and their self-management skills reinforced by strengthening HIV literacy across the continuum of care.
In many settings, optimizing the HIV care environment may be the most important action to ensure that there are meaningful increases in the number of people who are tested for HIV, linked to care, started on ART if diagnosed to be HIV positive, and assisted to achieve and maintain long-term viral suppression. Overcoming the legal, social, environmental, and structural barriers that limit access to the full range of services across the HIV care continuum requires multistakeholder engagement, diversified and inclusive strategies, and innovative approaches. Addressing laws that criminalize the conduct of key populations and supporting interventions that reduce HIV-related stigma and discrimination are also critically important. People living with HIV also require support through peer counseling, education, and navigation mechanisms, and their self-management skills reinforced by strengthening HIV literacy across the continuum of care.