Judging the epidemic has been prepared as a resource to help judges, magistrates, arbitrators and other judicial officers throughout the world adjudicate cases involving HIV-related issues. This handbook may also be used by judicial trainers and ministries of justice to deliver educational programmes to judges and magistrates on legal issues related to HIV and human rights. It may also be relevant to advocates, lawyers and other legal practitioners, and civil society organisations (including people living with HIV) that seek to gain specific understanding of HIV-related legal issues and the potential role of the courts in advancing human rights in the context of the epidemic. Based on international legal and human rights standards, the handbook contains examples of decided cases from different jurisdictions, good-practice advice and judicial rulings on HIV-related issues.
Uganda: New Anti-Homosexuality Bill a setback for Uganda’s HIV response
The draconian Anti-Homosexuality Bill passed by Uganda’s parliament on 20 December would deliver a major blow to the response to HIV/AIDS if it was enacted by President Yoweri Museveni, activists have warned.
Those found guilty of homosexual acts can be jailed for up to 14 years under the new law, a sentence that increases to life in “aggravated” cases, such as those committed by an HIV positive person, or those involving minors, the disabled and serious offenders.
Civil society activists fear that high-risk groups such as men who have sex with men (MSM) and sex workers – whose HIV prevalence is 13.7 and 33 percent respectively – will see their already limited access to prevention and treatment further eroded.
Amnesty International called the law “a grave assault on human rights [which] makes a mockery of the Ugandan constitution.
“President Museveni should avoid the trap of scapegoating a vulnerable minority in the interests of short-term political gain,” said Daniel Bekele, Africa director at Human Rights Watch.
“He should recognize that this repugnant bill is of no benefit to Ugandans – that it only serves to jeopardize basic rights – and reject it.”
The United States government has also called for the bill not to be enacted.
Canada: Study finds prisoners with unsuppressed viral loads nearly twice as likely to share used needles if they had been incarcerated
People living with HIV are more likely to share syringes and not disclose they are HIV positive when they are in jail, according to a new study by researchers at the B.C. Centre for Excellence in HIV/AIDS. The study, conducted between May 1996 and March 2012, involved interviews with 657 people who used injection drugs and were HIV-positive.
It found the participants spent approximately 15 per cent of that time in jail, and while in jail they had a detectable amount of HIV in their bloodstream 83 per cent of the time, which meant they could transmit the infection to others because they were not taking their medication as prescribed. That rate dropped to 62 per cent when they were not in jail and back on their medication.
The study also found prisoners with unsuppressed viral loads were nearly twice as likely to share used needles if they had been incarcerated. “There is absolutely no reason why incarcerated individuals should not receive the same level of medical care as those in the public,” said Terry Howard, director of community based research at Positive Living B.C. and former prison outreach program co-ordinator.
He estimates about 20 per cent of prisoners are HIV positive, but the majority don’t disclose while in prison because of the stigma and direct repercussions to them. As an example, Howard said, if prisoners are using drugs and sharing a needle with other inmates, they don’t want to have to wait to be the last person to use the needle, which would be the case if the others knew they were HIV positive. “I’ve also heard horror stories about them being beaten up (for being HIV positive) and stigmatized by guards who will make a big show of snapping on gloves when transporting prisoners who are HIV positive,” Howard said.
He said guards have argued against a needed distribution program, saying the syringes could be used as weapons against them, but Howard said there’s never been an incident of corrections staff being stabbed by a contaminated needle in those countries that do have a safe needle distribution program. “It’s a red herring they fly but the government buys it, and our government doesn’t want to tolerate drug use in prison,” Howard said.
African HIV criminalisation achievements and challenges highlighted at ICASA 2013
The African continent has more countries with overly broad and vague HIV-specific laws relating to HIV non-disclosure, exposure and/or transmission than any other global region, nearly all of which have been enacted in the past decade.
Although North America is the continent with the most known prosecutions, 26 African countries have overly broad and/ or vague HIV-specific criminal laws with a further three countries considering new HIV-specific criminal laws. This is worrying and disappointing given the growing evidence base and consensus of international agencies that such laws are counterproductive to HIV prevention efforts and generally fail to deliver ‘justice’.
Although there are few known prosecutions the majority of those prosecuted have been women – who are usually the first in a couple to know their HIV status due to routine antenatal testing and who are often erroneously accused of bringing HIV into a relationship.
In addition, South Africa recently prosecuted alleged criminal HIV transmission as attempted murder despite no evidence of intent to harm. (Read the judgement from the High Court of South Africa on alleged HIV exposure being attempted murder here.)
However, there have been some positive legal changes brought about by local advocacy supported by international civil society and UN agencies. Since 2010, at least four countries – Congo, Guinea, Senegal and Togo – have revised their existing HIV-related legislation or adopted new legislation that restrict use of criminal law to cases of intentional transmission.
And more recently advocacy in Malawi and Nigeria has resulted in the removal of overly broad HIV-specific criminal statutes from draft omnibus HIV Bills.
View the poster below or download the A4 double-sided printable version of the poster here.
Ruins: Chronicle of an HIV Witch-hunt
(53 min, Zoe Mavroudi, Greece, 2013)
Director Zoe Mavroudi’s powerful exposition of how HIV stigma was cynically used to scapegoat society’s most vulnerable. The film explores what happened in the run-up to the country’s 2012 national elections when a group of HIV-positive women were detained by the Greek police, forcibly tested, charged with a felony, imprisoned and publicly exposed, when their mug shots and personal data were published in the media.
More information at: http://ruins-documentary.com/en/
To support the women in their legal fight for justice please visit: http://ruins-documentary.com/en/donate/
Feature: ProPublica and BuzzFeed publish the most comprehensive article yet on HIV non-disclosure laws in the United States
Sex, Lies and HIV: When What You Don’t Tell Your Partner Is a Crime
by Sergio Hernandez, Special to ProPublica, Dec. 1, 2013.
This story was co-published with BuzzFeed.
[Un sommaire en français est aussi disponible ici]
Nick Rhoades was clerking at a Family Video store in Waverly, Iowa, one summer afternoon in 2008 when three armed detectives appeared, escorted him to a local hospital and ordered nurses to draw his blood. A dozen miles away, his mother and stepfather looked on as local sheriff’s deputies searched their home for drugs ó not illegal drugs, but lifesaving prescription medications.
Lab results and a bottle of pills found in the Rhoades’ refrigerator confirmed the detectives’ suspicions: Nick Rhoades was HIV-positive.
Almost a year later, in a Black Hawk County courtroom, Judge Bradley Harris peered down at Rhoades from his bench.
“One thing that makes this case difficult is you don’t look like our usual criminals,” Harris said. “Often times for the court it is easy to tell when someone is dangerous. They pull the gun. They have done an armed robbery. But you created a situation that was just as dangerous as anyone who did that.”
The judge meted out Rhoades’ sentence: 25 years in prison.
His crime: having sex without first disclosing he had HIV.
Officially, the charge, buried in Chapter 709 of the Iowa code, is “criminal transmission of HIV.” But no transmission had occurred. The man Rhoades had sex with, 22-year-old Adam Plendl, had not contracted the virus.
That’s not a surprise, because Rhoades used a condom.
And medical records show he was taking antiviral drugs that suppressed his HIV, making transmission extremely unlikely. A national group of AIDS public health officials later submitted a brief estimating that the odds of Rhoades infecting Plendl were “likely zero or near zero.”
After his lawyers petitioned the court, Rhoades’ prison sentence was changed to five years’ probation. But for the rest of his life ó he is 39 ó he will remain registered as an aggravated sex offender who cannot be alone with anyone under the age of 14, not even his nieces and nephews.
Rhoades’ is not an isolated case. Over the last decade, there have been at least 541 cases in which people were convicted of, or pleaded guilty to, criminal charges for not disclosing that they were HIV-positive, according to a ProPublica analysis of records from 19 states. The national tally is surely higher, because at least 35 states have laws that specifically criminalize exposing another person to HIV. In 29 states, it is a felony. None of the laws require transmission to occur.
Defendants in these cases were often sentenced to years ó sometimes decades ó in prison, even when they used a condom or took other precautions against infecting their partners. In 60 cases for which extensive documentation could be obtained, ProPublica found just four involving complainants who actually became infected with HIV. Even in such cases, it can be hard to prove who transmitted the virus without genetic tests matching the accused’s HIV strain to their accuser’s.
People with HIV have even done time for spitting, scratching or biting. According to the federal Centers for Disease Control and Prevention, spitting and scratching cannot transmit HIV, and transmission through biting “is very rare and involves very specific circumstances” ó namely, “severe trauma with extensive tissue damage and the presence of blood.”
Many law enforcement officials and legislators defend these laws, saying they deter people from spreading the virus and set a standard for disclosure and precautions in an ongoing epidemic.
“Shifting the burden of HIV disclosure from the infected person, who is aware of a known danger, to one who is completely unaware of their partner’s condition smacks of a ëblame the victim’ sort of mentality,” Jerry Vander Sanden, a prosecutor in Linn County, Iowa, wrote in an email to ProPublica. “It would be like telling a rape victim that they should have been more careful.”
Even many people with HIV support the laws. In a recent survey of HIV-positive people in New Jersey, 90 percent said that people with the virus bore most of the responsibility to protect their partners. More than half approved of the kind of laws that resulted in Rhoades’ sentence.
But some health and legal experts say using criminal penalties to curtail the epidemic could backfire and fuel the spread of HIV. According to the CDC, 1.1 million Americans are currently living with HIV, but one-fifth of them don’t know it. And studies show that about half of newly infected people got the virus from those who didn’t know they had HIV. So relying on a partner to know, let alone disclose, their HIV status is a risky proposition.
The laws, these experts say, could exacerbate this problem: If people can be imprisoned for knowingly exposing others to HIV, their best defense may be ignorance. Such laws, then, provide a powerful disincentive for citizens to get tested and learn if they carry the virus.
The laws “place all of the responsibility on one party: the party that’s HIV-positive,” said Scott Schoettes, a lawyer who supervises HIV litigation for Lambda Legal, a national gay-rights advocacy group. “And they lull people who are not HIV-positive ó or at least think they are not HIV-positive ó into believing that they don’t have to do anything. They can just wait for their partner to reveal their status and not, instead, take steps to protect themselves.”
Schoettes also says that the laws unfairly single out HIV, further stigmatizing and reinforcing misconceptions about living with the virus.
“There’s no reason why we should be singling out HIV for this kind of treatment,” he said. “It’s based in just a lot of fear and misconception.”
Being HIV-positive can still carry a powerful stigma. Since July 2010, the U.S. Department of Justice has opened at least 49 investigations into alleged HIV discrimination. The department has won settlements from state prisons, medical clinics, schools, funeral homes, insurance companies, day care centers and even alcohol rehab centers for discriminating against HIV-positive people. Individuals with HIV may also fear that news of their status will spread to third parties, leading to rejection, embarrassment or ostracism for themselves or even their loved ones.
In September, a disability rights group accused the Pea Ridge, Ark., school district of kicking out three siblings after officials learned that members of their family had HIV. The family’s lawyers declined to comment. The school district did not respond to requests for interviews but issued a statement acknowledging that it had “required some students to provide test results regarding their HIV status in order to formulate a safe and appropriate education plan for those children.”
In romantic or sexual settings, people with HIV often report fear of rejection, abandonment and stigmatization.
“My first girlfriend in middle school ó her mom banned her from seeing me, and it took me five years before I felt comfortable to try again,” said Reed Vreeland, a 27-year-old New Yorker who was born with HIV. Vreeland works as the communications coordinator for the Sero Project, a nonprofit advocacy group that campaigns against HIV exposure laws, which it denounces as “HIV criminalization.”
In 2006, Vreeland started dating a classmate at Bard College in upstate New York. He disclosed his HIV status on their second date.
“What’s going through your head is being scared of being rejected,” he said. “It’s scary to give someone that power.”
Vreeland and his girlfriend continued to date. Last spring, they married at a ceremony in the Bronx. “It took me a long time to propose, because I thought I would die,” he recalled. “I was saying, ëWell, OK, why should I propose if I’m scared of dying in 10 years? And if we do have a kid, then I might die and leave my kid without a father, like I grew up without a mother.'”
The fear is “choking” and “silencing,” he said. “You’re conscious that saying three letters will change the way people will see you.”
In some cases, people with HIV have been met with violence ó and even death ó after disclosing their status. Last month, in Dallas, 37-year-old Larry Dunn was sentenced to 40 years in prison for murdering his HIV-positive lover. Police said he used a kitchen knife to stab and kill Cicely Bolden, a 28-year-old mother of two, after she told him about her HIV status. “She killed me,” he told investigators, according to his arrest warrant, “so I killed her.”
Until recently, criminal punishment was virtually unheard of for infectious diseases other than HIV. Federal and state officials have the authority to quarantine the sick to contain epidemics, but this power was typically granted to health authorities, who are versed in the latest science, not police and prosecutors. Very few criminal statutes take aim at diseases. At least two states have catchall laws against exposing others to “communicable diseases,” but only if exposure happens through routes most commonly associated with HIV, such as sex, sharing needles or donating blood. And while some states have laws that specifically punish exposure to tuberculosis, syphilis or “venereal diseases,” HIV exposure is almost always punished more severely.
But since 2007, three states have added hepatitis B and C to laws criminalizing HIV exposure. Those diseases are most prevalent among the same groups of marginalized people most at risk for HIV: intravenous drug users; gay men, especially those who are black or Latino; and black women.
Yet the laws may be unnecessary. In rare cases when someone intentionally tries to spread a virus, prosecutors have been able to put them away using ordinary criminal laws, such as assault or reckless endangerment. In 1997, a New York man named Nushawn Williams was accused of deliberately infecting at least 13 people, including two underage girls, with HIV. Williams pleaded guilty to two counts of statutory rape and one count of reckless endangerment. When his 12-year sentence ended in 2010, state officials kept him confined under laws that allow dangerous psychiatric patients to be locked up. He remains behind bars.
In Iowa, Rhoades’ case has prompted some lawmakers to reconsider whether exposing someone to HIV should carry such a heavy punishment.
“Putting somebody in prison for 25 years when they didn’t even transmit HIV is the most absurd thing that the state could be doing,” said Matt McCoy, an Iowa state senator who has introduced legislation to reduce the penalties. “It’s medieval.”
Even Plendl, the man Rhoades had sex with, thinks the law is too harsh. “Do I think he needs to be locked up forever?” Plendl asked. “No. Do I think these laws need to be revisited? Yes.”
* * *
In 1986, scientists had just christened the virus that causes AIDS, the human immunodeficiency virus, or HIV. The government had already logged more than 16,000 AIDS cases and 8,000 deaths since the American epidemic began, mostly among gay men and drug users. At the time, not a single drug was approved to target HIV, and the diagnosis was, for many, a death warrant.
In a panic, state lawmakers across the country ó starting with Kernan “Skip” Hand, a Republican state legislator from Jefferson Parish, La. ó began to take a law-and-order approach to keeping HIV out of their communities.
Hand’s bill, the first of its kind in the country, passed in 1987. It imposed a sentence of up to 10 years in prison and a $5,000 fine on anyone who “intentionally” exposed a person to HIV without their “knowing and lawful consent.”
The next year, Georgia adopted a statute that made no mention of intent; it could be applied to anyone who did not disclose their HIV status before having sex or sharing needles.
Weigh In: Do HIV Laws Protect or Persecute?
In 1989, the American Legislative Exchange Council, or ALEC ó a conservative nonprofit that develops policy positions and drafts model bills for state legislatures ó assembled a special HIV task force, which published a set of prototype statutes on subjects ranging from mandatory testing to insurance coverage. Buried in Chapter 6, alongside a proposed emergency quarantine law, was a single-page bill called the “HIV Assault Act,” which became the template for state HIV exposure laws for the next decade.
Alan Smith, who served on the committee that drafted ALEC’s model HIV bills and later served as ALEC’s executive director, recalled members’ concerns that people might intentionally try to spread the virus to drive more funding toward medical research.
“I guess there was a worry that there would be a lot worse disease than it could’ve been if people were actually on a mission to make sure more people got it so more research money could be devoted to curing it,” Smith said.
A turning point came in 1990, when Congress inadvertently gave the criminalization effort a boost by passing the Ryan White CARE Act, a landmark law that funded HIV/AIDS services.
In the run up to passage, Jesse Helms ó the late Republican senator from North Carolina ó proposed an amendment that would have criminalized HIV-positive health care workers who failed to disclose their status to patients and made it a federal crime for anyone with HIV, as well as anyone who had ever used injection drugs or engaged in prostitution, to donate, sell or attempt to donate or sell blood, semen, tissues, organs or bodily fluids. (The act itself was named after a hemophiliac teenager from Indiana who became a national poster child for the AIDS crisis when he was expelled from middle school after contracting HIV from a tainted blood treatment.)
But Ted Kennedy, the late Democratic senator from Massachusetts and the act’s primary sponsor, offered an alternative: Defund services unless states passed legislation to safeguard their blood and organ donation networks.
“No state,” Kennedy said from the Senate floor, describing the compromise amendment, “could receive funds under the act, unless laws are in place to prosecute a person who donates blood or organs if one knows that he or she is infected with the HIV virus and knows the risk of transmission from making such a donation.”
Waiting in the wings was the ALEC bill, which outlawed blood and tissue donations by people with HIV and also made it a crime for anyone with HIV to have “intimate contact” with another person without first disclosing his or her HIV status. By 1993, versions of the HIV Assault Act had been passed in Florida and introduced in Iowa, Michigan, Mississippi, New York, Nevada, Tennessee and Virginia. By the end of the decade, copycat bills had passed in nine states, including Iowa, which enacted its law in 1998.
A side-by-side comparison shows that the Iowa law was almost identical to ALEC’s HIV Assault Act. Iowa’s only major change was to its name: The “HIV Assault Act” became the “Criminal Transmission of Human Immunodeficiency Virus” law, itself a misnomer because transmission isn’t necessary for the charge to stick.
When Congress reauthorized the Ryan White CARE Act in 2000, it dropped the criminalization provision for blood and tissue donations. Nevertheless, since then, at least 14 bills have been passed across the country either enacting new HIV exposure laws or toughening existing laws’ penalties, especially when the victim is a police or corrections officer.
In 2011, for example, Nebraska passed a measure that made biting or spitting on public safety officers a misdemeanor punishable by one year in jail and a $1,000 fine ó unless the offender is HIV-positive. Then the same crime is a felony punishable by up to five years in prison and a $10,000 fine.
At the same time, three states ó Mississippi, Nebraska and Tennessee ó have criminalized exposing someone to hepatitis B or C. In Nebraska and Tennessee, this is a misdemeanor, while HIV exposure is a felony, even though, according to the World Health Organization, hepatitis B is up to 100 times more infectious than HIV.
* * *
On June 26, 2008, Nick Rhoades was at home in Plainfield, Iowa, when he received a chat invitation on Gay.com, a dating and social networking site. The sender, Adam Plendl, was a 22-year-old student at the University of Northern Iowa.
At 3 that morning, the men struck up a conversation. Plendl invited Rhoades to meet him in Cedar Falls, roughly 30 miles south of Plainfield, where Plendl had just moved into a new apartment several blocks from campus. The two men spent the next several hours drinking pomegranate vodka martinis, smoking marijuana, unpacking Plendl’s belongings and bonding over their struggles with bipolar disorder. Eventually, they had sex.
A few nights later, Plendl was sharing a midnight cigarette with Jordan Brown, a friend who had learned through the grapevine that Rhoades was, as he later described it to police, “sick.” Plendl panicked at the possibility that he had been exposed to HIV. He said he “flew out of the house” to the emergency room of the nearby Sartori Memorial Hospital.
As he tells it, Plendl never planned to press charges against Rhoades. He went to the hospital seeking a doctor who could prescribe him a short-term, emergency regimen of HIV drugs that, if started within 72 hours of exposure to the virus, can stop infection from taking root. But when the Sartori staff seemed clueless about the procedure, Plendl went to the emergency room at Covenant Medical Center in the neighboring town of Waterloo.
There, Brandy Weida-Cooper, a registered nurse who was working the graveyard shift, admitted Plendl to the ER and, records show, made the call to involve police. “I never called the police,” Plendl said. “Yes, when I was asked questions, I provided them answers. But I did not call the police; the hospital did.”
In a telephone interview, Weida-Cooper declined to explain what spurred her decision to alert authorities. (A spokesman for Wheaton Franciscan Healthcare, the Roman Catholic nonprofit that owns both Covenant and Sartori, also declined to comment.) In any case, by 4:02 a.m., a Cedar Falls patrol officer was standing in Weida-Cooper’s emergency room, ready to take Plendl’s statement.
* * *
The more than 500 instances documented by ProPublica in which people have been convicted of or pleaded guilty to HIV-specific laws since 2003 represents one of the largest collections of such cases ever assembled. Still, it is almost certainly a substantial undercount.
The data was drawn from more than 1,300 records, including court files, police reports and registries of sex offenders and prisoners. Some law enforcement agencies refused to provide records about their cases or redacted names and case numbers, saying that the suspects’ HIV status ó once used to prove their criminal guilt ó should be protected out of concern for their medical privacy. (A full breakdown of the data is here.)
Some of the cases were originally compiled through public records requests made by the Sero Project; most were independently obtained by ProPublica.
Despite its limitations, the material creates a rough portrait of how these laws have been applied through the years.
ProPublica was able to find just four cases that involved lawmakers’ original concerns about protecting the blood and organ supply. Two of these four resulted in a conviction or guilty plea, one was dismissed, and the outcome of the last could not be determined.
For cases in which the route of potential transmission could be determined, the overwhelming majority involved sex. The circumstances and relationships in those cases confound stereotypes or preconceived notions: HIV-positive defendants and their accusers have included gay and straight couples in one-night stands, dating relationships or even years of marriage. Cases have involved instances of sex between prisoners, rape and child abuse.
In Waterloo, Iowa, 42-year-old Donald Bogardus, a church-going, HIV-positive gay man who also suffers from cerebral palsy, recently pleaded guilty to charges of failing to disclose his status to a partner. “I wanted to tell him, but when I went to say it, I clammed up,” Bogardus told the Daily Iowan last year. “So many things came across my mind. I was afraid he was going to blab it out to everybody. But I still regret not telling him. I really do.”
Bogardus currently works as a nurse’s assistant, but his guilty plea will place him on the state’s sex offender registry, barring him from working with patients in nursing homes.
Even just the fear of prosecution has had consequences for people with HIV. In New York, one HIV-positive woman interviewed by ProPublica said she didn’t report being raped because her attacker threatened to press charges for not disclosing her status. (New York does not have an HIV disclosure law, but the woman said she didn’t know that and feared prosecution because she’d heard of cases elsewhere.)
Women, including many alleged sex workers, were the accused in almost a quarter of the convictions and guilty pleas for which gender could be determined.
In St. Louis, Nigaila Gibbs was 20 years old when police arrested her during an undercover sting operation in 2010. Gibbs, who was born with HIV, began prostituting herself after aging out of Missouri’s foster care system. Police accused her of having sex with “hundreds” of clients and failing to warn them about her HIV status, although Gibbs told police she always practiced safe sex. At the time of Gibbs’ arrest, St. Louis County police encouraged potential victims to come forward. Three clients stepped up to complain about Gibbs, but a police spokesman said no one was found to be infected or charged with soliciting a prostitute.
Gibbs ultimately pleaded guilty to “performing an act of prostitution” while knowingly infected with HIV and was sentenced to five years in Missouri state prison. Today, searching for her name on Google turns up blog posts and message board threads titled “AIDS Whore Nigaila Gibbs May Have Infected Hundreds!” and “Fat ugly prostitute infects over 100 clients w/ HIV.”
In one 2006 case, the defendant was already in prison when he was charged with an HIV-related offense.
Thomas Tompkins was serving his last month in prison at Ohio’s Richland Correctional Institution when a guard caught him performing oral sex on another inmate in the prison library. State police questioned the two inmates about whether the encounter was consensual, and both men agreed it was. But when Tompkins acknowledged that he had not disclosed his HIV-positive status to the other inmate, prosecutors accused him of felonious assault with HIV.
Scientists agree that a man who receives oral sex has virtually zero chance of contracting HIV.
Still, Tompkins pleaded guilty to a reduced charge of aggravated assault, adding an extra year to his sentence.
And in a 2010 case from South Carolina, a 32-year-old man named Jesus Cazares spent five months in the Marion County jail awaiting trial for “exposing another to HIV.” He pleaded guilty and was credited with time served, but not before U.S. Immigrations and Customs Enforcement filed to detain him on immigration charges. In February 2011, Cazares was released into ICE custody, and a federal judge ordered him “removed” to Mexico.
In addition to the convictions and guilty pleas, ProPublica found at least 179 instances in which people were acquitted or had their cases dismissed. Yet even then, the repercussions can be severe. The accused can find their names splashed in local news accounts, making their HIV status common knowledge; they can lose jobs, homes, family members and friends; and if they can’t make bail, they can be stuck in jail, where inmates can face spotty access to HIV medications and other problems.
Last year, St. Louis prosecutors accused 40-year-old Adam Childs of exposing an ex-boyfriend to HIV. While awaiting trial in the city jail, records show, Childs was raped by another inmate and moved to protective custody. A few months later, a nurse and a prison guard were dispensing medications in Childs’ cell block when they found his lifeless body hanging over the stainless steel toilet in his cell, strung from a sprinkler cover with a blue, standard-issue jail bed sheet.
* * *
One consequence of the viral exposure legislation is that public health activities and law enforcement, which have traditionally been kept separate, can now overlap. In some states, such as Mississippi, people who test HIV-positive are routinely asked to sign a document called a “Form 917.” By signing it, patients acknowledge they have been counseled about the basics of living with HIV, including the legal consequences of not telling partners they have the virus. Similar forms have also been used in Arkansas, Michigan and North Dakota.
In several states, including Idaho, Missouri, Indiana, Michigan and Iowa, ProPublica found, prosecutors and judges have used subpoenas and warrants to force health officials to hand over these forms along with other medical records, such as test results, as evidence against patients charged with violating viral exposure laws. County prosecutors in Indiana, for example, have served at least 20 such subpoenas to the state health department since 2010.
Sometimes, health officials have initiated criminal proceedings. In Grand Traverse County, Mich., former county health officer Fred Keeslar sent a memo to the local prosecutor headlined “Recalcitrant Behavior,” suggesting that police set up a sting operation to arrest and prosecute an HIV-positive man suspected of cruising for sex in public bathrooms without disclosing his status. Keeslar did not respond to requests for comment.
On the federal level, Obama administration officials have come out against HIV-specific criminal laws. In 2010, the White House’s Office of National AIDS Policy issued a white paper saying that the “continued existence and enforcement of these types of laws run counter to scientific evidence about routes of HIV transmission and may undermine the public health goals of promoting HIV screening and treatment.” The Presidential Advisory Council on HIV/AIDS has also condemned these laws.
In 2011, the National Alliance of State and Territorial AIDS Directors, or NASTAD, also endorsed the repeal of laws that criminalize HIV exposure or nondisclosure. (Last June, NASTAD also filed a friend-of-the-court brief in the Rhoades case.)
But across the states, health officials have varying opinions. “The existence of the statutes does not affect our prevention, diagnosis and treatment efforts,” a spokesman for the Virginia state health department said.
But Jill Midkiff, a spokeswoman for Kentucky’s Cabinet for Health and Family Services, said that “imposing harsher sentences on individuals with HIV or treating HIV-positive patients differently in the eyes of the law may impact the effectiveness of the Department of Public Health’s HIV prevention efforts.”
And Donn Moyer, a spokesman for the Washington State Department of Health, said, “we believe it’s time to look at the effectiveness of such laws, given current knowledge and understanding of HIV transmission and treatment, which have advanced a lot since most of those HIV laws were written.”
Officials in Louisiana did not comment on specific criticisms of its law, but internal emails discussing ProPublica’s questions show how sensitive the topic can be. One former health department spokeswoman told a colleague it is “a touchy topic that will require governor’s office involvement.”
In Tennessee, ProPublica’s questions were sent to the state epidemiologist, who told a spokesman: “Ain’t touching it with a 10 foot pole.”
In Iowa, the Rhoades case helped spur a bill that would lower the penalties for HIV exposure, but it failed to pass. Its lead sponsor said he plans to reintroduce it. For anyone who intentionally tried to infect someone, the punishment would remain harsh: 10 years if infection occurred, and five years if it didn’t. In cases where someone didn’t intend to infect his partner but still did so after failing to take “practical means to prevent” transmission, the penalty would be two years. If there was no intention to infect and no one was infected, there would be no penalty. Local AIDS activists and the state health department support the bill, but some prosecutors still oppose it.
* * *
Whether Adam Plendl actually faced a significant risk for contracting HIV from Rhoades, or was even exposed to the virus during their encounter remains unclear. HIV is far less transmissible than many other sexually transmitted infections, such as herpes. Even for unprotected anal sex, the riskiest sexual act, the receptive partner’s chances of contracting HIV have been estimated at only five in 1,000. (The insertive partner is at a much lower risk.)
The men agree that Rhoades wore a condom during intercourse, although Plendl claims it fell off. Neither man recalls whether Rhoades ejaculated during the encounter.
But Rhoades was taking a cocktail of three antiretroviral drugs, and his medical records show they were working. The drugs had suppressed the amount of HIV in his blood to such minute levels that it was undetectable in lab tests. A widely heralded 2011 study found that similar patients were 96 percent less likely to pass HIV on to a partner.
The men did not use a condom when Plendl performed oral sex on Rhoades, and prosecutors later argued that the act could have exposed Plendl to pre-seminal fluid containing HIV. While HIV transmission from oral sex has been documented, the CDC says it’s rare, and it considers the risk low. Plendl later said he was suffering from a shaving nick, which, he worried, could have made him more susceptible to transmission.
Lab results eventually confirmed that Plendl did not contract HIV.
In the days after he visited the emergency room, Plendl cooperated with Mark Abernathy, the Cedar Falls detective who was assigned to investigate the case. Plendl gave Abernathy a copy of Rhoades’ Internet profile, which listed his HIV status as negative.
In an interview, Plendl told ProPublica he asked Rhoades if he was “clean.” He explained, “I always ask anyone, before anything, ëIs your profile correct with your HIV status?'”
Rhoades said he doesn’t remember that exchange, but he admitted to lying about his HIV status online.
“That was different,” he told a prosecutor in 2011. “That was a public openness.” Telling his close friends and family was one thing, Rhoades said, but he didn’t want his HIV infection available to “people who randomly page through profiles on an online website.”
“It’s a stigmatized condition,” he added. “I have a job.”
After their encounter, Rhoades left several voicemails on Plendl’s phone. “I wanted to get together with him,” Rhoades said in an interview. “I wanted to sit down and have the conversation about my HIV status. I didn’t realize that the reason he wasn’t returning my phone calls was because he was already in contact with law enforcement.”
Plendl said he finally called Rhoades back, with his phone wired up to police recording equipment. He confronted Rhoades, who confirmed, on tape, that he was HIV-positive and that the men had engaged in unprotected oral sex during their encounter. The recording would become crucial evidence.
Four days later, on July 14, a Black Hawk County judge approved Detective Abernathy’s request for a search warrant, allowing him to seize Rhoades’ medical records, prescriptions and a sample of his blood.
“They came to my work,” Rhoades said. “I think it was three openly-armed police detectives from an adjacent city.” The officers, he continued, “asked me to go down to the local sheriff’s office and discuss something with them, and they didn’t say what this was about.”
At the sheriff’s station, Abernathy led Rhoades ó who was dressed in a striped blue polo shirt, light tan khakis and a pair of white sneakers ó to an interview room. Initially, Rhoades signed a Miranda waiver, acknowledging his rights to silence and legal counsel, while Abernathy, a tall, balding man in his early 40s, questioned him about the encounter with Plendl.
“I have a case involving you and an Adam Plendl,” Abernathy said. “Do you know who Mr. Plendl is?”
“I know someone named Adam,” Rhoades replied.
The detective continued, asking how, when and where the meeting with Plendl occurred.
“I’m not trying to make you uncomfortable,” Abernathy said.
“I’m a little uncomfortable,” Rhoades replied.
“What was the intent of the meeting, if you will?”
“It was purely social. And I don’t know if you can subpoena ó I don’t know if they keep records of those chat conversations, but if they do, I’d be more than willing to share them, because I was quite clear that it was just a social nature,” Rhoades said.
As the interrogation continued, Rhoades plainly told Abernathy about his HIV status and his phone conversation with Plendl ó which, unbeknown to Rhoades, the detective had already listened to.
“He did find out that I’m HIV-positive,” he told the officer, “and he was very concerned about any interaction that he had with me, and I tried to assure him that nothing that happened between us was anything of risk.”
“You said you’re pretty open with it,” Abernathy said. “You don’t advertise it, but you tell your friends?”
“It’s too much to stress about. It’s a bad thing, but the more open I am, the less anxious I feel. And people around me that I’m close to ó I think it helps our friendship to be honest.”
“How come you didn’t let Adam know?” the detective asked.
“Again, it’s a need-to-know basis. And there was no ó ”
“But you guys had sex?”
“No.”
“You did not have sex?”
“We did not have sex.”
Abernathy had caught Rhoades in a lie, and he bore down on it.
“Are you saying there was no oral or anal penetration?”
“No,” Rhoades answered. “No.”
“You look surprised. Which one of those surprised you?”
“Well, they both surprise me. With my condition I have to be pretty ó picky, I guess, about who I’m with and why I’m with them,” Rhoades said. “I’m honest about it. Especially when it comes to a situation that would lead to possibly a sexual encounter.”
Abruptly, Abernathy excused himself from the interrogation room. It wasn’t until he returned ó and revealed to Rhoades that his phone call with Plendl had been taped ó that Rhoades realized how serious the situation had become. He invoked his right to a lawyer, ending the interview, and went with the cops to a local hospital where nurses drew his blood.
When he was finished, he told his mother, “I don’t know if I’m going to be in trouble.”
* * *
After Rhoades’ police interrogation, his parents found him a lawyer: James Metcalf, a former local prosecutor who now runs his own criminal defense practice in downtown Waterloo.
As the case progressed, Rhoades pleaded with Plendl not to press charges. After the police interview, he left a final voicemail on Plendl’s phone, begging him to abandon the case.
“I’m just calling to absolutely get on my knees and beg you to please drop these charges,” Rhoades urged. “This has all just gone absolutely crazy. Please consider ó again, I absolutely beg you, beg you, beg you to please drop these charges.”
But on July 28, Abernathy submitted a criminal complaint to the court and county prosecutors, accusing Rhoades of violating the state’s HIV exposure law. A judge issued an arrest warrant.
When police showed up to take Rhoades into custody, he was nowhere to be found. “Without getting into too much detail, I had a nervous breakdown,” he said.
In an affidavit later submitted to the court on Rhoades’ behalf, Colleen Brems, a nurse who treated him at the University of Iowa Hospitals and Clinics in Iowa City, said that he had been admitted to the hospital’s mental health unit to recover “from a suicide attempt in [the] context of [a] severe depressive episode.”
“In a small community like Iowa,” Rhoades explained, “dealing with the most stigmatized condition, in my mind, that currently exists; becoming fodder for the media gossip mill; me and my HIV status becoming public domain; and the idea of, you know, becoming a felon and having the embarrassment to my family and feeling like my life would be absolutely ó there would be no life after if this prosecution were successful.
“It was more than I could take, and I just ó I crumbled.”
Rhoades spent a month in inpatient care. When he was discharged on Sept. 30, 2008, he was immediately taken into custody and escorted to the county jail in Waterloo. “I walked out of the hospital in my cuffs and shackles,” he recalled.
Rhoades pleaded not guilty, and the judge set his bond at $250,000. Rhoades said his family “didn’t have that kind of cash,” so he spent seven months in the Black Hawk County jail, waiting for trial.
For the first 20 days, the sheriff’s office said, Rhoades was placed in solitary confinement and was allowed one 30-minute visit each week. He lived in the jail’s secured housing unit, or SHU (pronounced “shoe”), where his HIV medications were delivered through a slot in the cell door.
Eventually, Rhoades was transferred to a cell in the jail’s high-security wing. He left the jail twice, the sheriff’s office said, for medical appointments, where he sat in a waiting room wearing an orange jumpsuit, leg irons and handcuffs.
In the meantime, Metcalf had suggested that Rhoades waive his right to a speedy trial so he would have more time to prepare a defense. At one point, Metcalf started deposing Plendl, but the interview was never completed.
By May 2009, Rhoades had grown exhausted and frayed from jail and the uncertainty. He and Metcalf decided to enter a guilty plea and hope for a lenient sentence. But at the hearing, Judge Harris gave Rhoades the maximum sentence under Iowa’s law ó 25 years in state prison. The maximum sentence under Iowa law for sexually abusing a child is 10 years.
“Prison very rarely provides rehabilitation,” Harris told Rhoades. “You’re being sent there as a punishment.”
* * *
Harris’ decision to give Rhoades the maximum sentence immediately caught the attention of the local news media. “I got lots of mail,” Rhoades recalled. “I got mail from friends, family. I got mail from POZ magazine” ó a monthly publication for people with HIV/AIDS. “I got mail from supporters who didn’t even know me.”
Judge Harris was also getting mail. Over the summer, he received a letter from Jeanne Brager, a friend of Rhoades’ who lived in Modesto, Calif., urging the judge to modify the sentence. “Murderers and child rapists receive less time than this young man did,” Brager wrote. “He is not a man with a criminal mind. Prison will destroy him. He has far too much goodness and sensitivity to survive in such surroundings. He will simply wither away and die.”
Harris also heard from Mark Kassis, an HIV/AIDS advocate in Ames, Iowa, who argued that jailing people with HIV for failing to disclose their status set a dangerous precedent and would “deepen the stigma around the disease” that “actually leads to the spread of HIV.”
The letters seemed to work. A few months later, Rhoades got a call from his attorney. “Judge Harris approached him and said, ëNow would be a good time to apply for that [sentence] reconsideration,'” Rhoades recalled. “Judge Harris said, ëYou apply for it, I’m going to grant it.'” (Harris declined to comment for this article.)
On Sept. 11, 2009, Harris granted Rhoades’ application for a sentence reduction, lowering his sentence to five years of supervised probation. Rhoades, who now lives in Waterloo, must obey an 11 p.m. curfew, wear a GPS monitoring bracelet, cannot use social media sites such as Facebook or Twitter, cannot drink alcohol and must obtain permission from a probation officer to leave the county, even to visit his parents in nearby Plainfield. He remains a registered sex offender and, as a convicted felon, he cannot vote.
Around the time that Rhoades’ sentence was reduced, Sean Strub, a fellow Iowan, was wading into the debate over HIV exposure laws. Strub, a tall, wiry 55-year-old is a well-known AIDS activist and the founder of the Sero Project and POZ magazine. In 1985, Strub was living in New York City when he was diagnosed with HIV. He nearly died in the mid-1990s, until a daily regimen of 18 pills turned his health around.
When Strub learned about Rhoades’ case, he introduced him to a civil rights attorney named Dan Johnston. In 1969, a young Johnston was working with the American Civil Liberties Union when he won Tinker v. Des Moines, a landmark U.S. Supreme Court case that established free speech rights for students in public schools. Johnston, who happened to be planning a visit to Iowa that weekend to celebrate Tinker‘s 30th anniversary, agreed to meet with Rhoades and Joseph Glazebrook, a gay 29-year-old attorney based in Des Moines.
Glazebrook had worked closely with HIV-positive clients, but mostly on employment discrimination cases. “When I first got the case, I probably was not the most sympathetic person on this issue,” Glazebrook recalled. “I guess my uninformed opinion was probably rooted in the assumption that it’s never OK to have sexual relations with somebody without disclosing things about you that could hurt them,” he said.
But as he worked on the case, his position shifted.
“Even if it’s the moral thing to do ó to be open and honest with your sexual partners about any threat to your sexual partner ó that may be a very legitimate and moral position to take, but it doesn’t make sense to legislate based upon that particular thought or feeling,” he said.
In 2010, Glazebrook and Johnston filed a petition in Black Hawk County court seeking post-conviction relief, alleging that Rhoades’ original defense lawyer had failed to fully investigate the case; that Rhoades did not understand what he was pleading guilty to; and that there wasn’t enough evidence to sustain the charges in the first place. (Metcalf, Rhoades’ original defense attorney, did not respond to requests for an interview.)
According to Rhoades’ appellate lawyers, the fact that he used a condom was proof that he did not intend to expose Plendl to HIV. In fact, they argued, wearing a condom suggested the opposite: Rhoades was trying to protect Plendl.
But Iowa’s law, which bans “the intentional exposure of the body of one person to a bodily fluid of another person in a manner that could result in” HIV transmission, doesn’t make an exception for safe sex. Rhoades hadn’t disclosed that he has HIV, so, the state argued, the “wrongful act is engaging in a sex act in a manner through which the virus could be transmitted.” It didn’t matter whether Rhoades used a condom, intended to expose or infect Plendl or even whether infection was likely. “Any kind of act in which a potential exchange of fluids exists is the kind of act that is criminalized by the statute,” the state said.
In 2011, just before Christmas Eve, county Judge David Staudt denied Rhoades’ petition, writing that his attorney had fully explained the statute and that Rhoades was “a very knowledgeable individual concerning the transmission or potential transmission of bodily fluids and its importance in the possibility of transmitting the HIV virus.”
The Iowa Supreme Court declined to hear another appeal but transferred the case to the state’s Court of Appeals, an intermediate-level court. In October, that court published a 3-0 ruling, upholding Rhoades’ conviction.
In an eight-page opinion, Judge Richard Doyle said Rhoades exposed Plendl to bodily fluids during the unprotected oral sex. Quoting earlier testimony from Rhoades’ doctor, the court concluded that although infection through unprotected oral sex is unlikely, it is still “possible,” and the conviction should be upheld. (Rhoades’ lawyers pointed out that Plendl was only exposed to Rhoades’ pre-ejaculate. In its friend-of-the-court brief, NASTAD called the risk of transmission in Rhoades’ case “likely zero or near zero,” while his doctor pegged the chance of transmission at one in a million.)
Rhoades’ lawyers, including Scott Schoettes, the Lambda attorney, are now asking the state Supreme Court to reconsider the appeal. While he does not have any more prison time to serve, Rhoades’ conviction under the state’s HIV exposure law makes him a “Tier III” sex offender for life. This designation groups Rhoades with the worst of the worst ó “sexually motivated” killers and kidnappers, child molesters, rapists and sex traffickers.
Every six months, at a small, nondescript office building across the Cedar River from downtown Waterloo, a polygraph examiner is brought in to conduct a “maintenance examination,” in which Rhoades must answer a series of questions about his sex life: “Have you ever had any sexual activity with an animal?” “Have you worn female clothing during masturbation?” “Have you ever had sexual contact with a corpse?”
Over the summer, while the court’s decision was still pending, I received an email from Rhoades, sent from the psychiatric unit at the University of Iowa Hospitals and Clinics. A few days earlier, Rhoades said, he had attempted suicide, fashioning a belt into a makeshift noose and swallowing a mixture of anti-seizure drugs and sleeping pills.
For four weeks, Rhoades said, he was hospitalized as doctors worked to rein in his moods using Lamictal, a drug typically used to treat bipolar disorder and seizures. At one point, he recalled, his mood swings became so severe that his doctors began to consider electroconvulsive therapy ó shock treatment.
“I’m either going to live and somehow make it and thrive ó OR I’m going to fucking put on my best face and charm my way out of here and who knows what will happen then,” he wrote from the hospital.
On July 3, I received another email. Rhoades’ mood had improved to the point that doctors were ready to let him go, with “pretty intensive outpatient follow-up.”
The next day ó exactly five years and one week after his encounter with Adam Plendl ó the doctors sent Rhoades home.
His nurse, he wrote, had “convinced them that I am not an imminent danger to myself or anyone else.”
When I asked if he considered himself dangerous, he wrote back:
“I’m never a danger to anyone else.”
A critical summary of recently presented/published social science research into the impact of overly broad HIV criminalisation
In recent years, the criminalization of HIV transmission, exposure and non-disclosure has become a hot topic among those working within the global AIDS milieu. Social scientists have become increasingly attentive to the complex and varied consequences and impacts of HIV criminalization.
Experts agree: overly broad HIV criminalisation is doing more harm than good
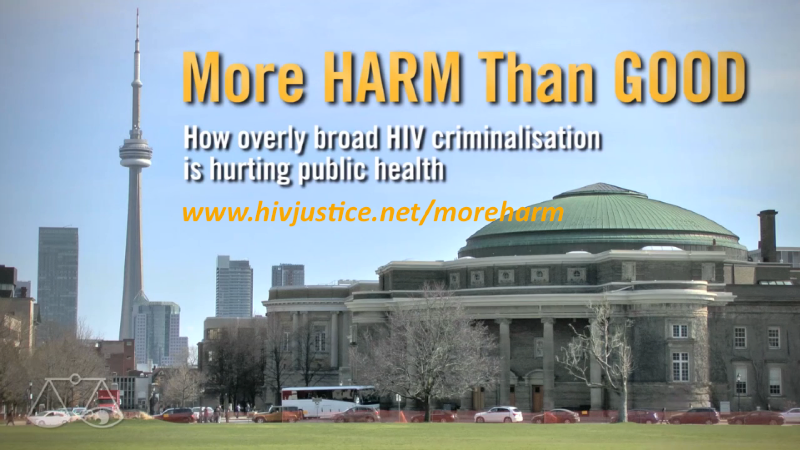
The HIV Justice Network has today released a new documentary, More HARM Than GOOD: How overly broad HIV criminalisation is hurting public health which had its world premiere at the US Conference on AIDS in New Orleans on September 10th. We hope it will be useful for both education and advocacy. To watch the video and to see all the studies cited in the documentary, visit www.hivjustice.net/moreharm. Download the video from our Vimeo channel: www.vimeo.com/hivjustice/moreharm
In many countries around the world, people with HIV are being made criminally liable for HIV prevention.
Despite strong recommendations against this overly broad use of the criminal law by UNAIDS and the Global Commission on HIV and the Law, the latest report from the Global Network of People Living with HIV and the HIV Justice Network highlights that new laws continue to be proposed and enacted, and more prosecutions are taking place than ever before.
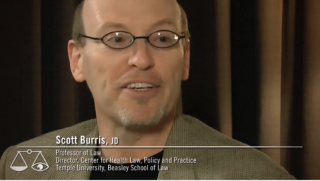
The most commonly cited rationale of the criminal law is to deter morally unacceptable behaviour through fear of punishment. Scott Burris and Zita Lazzarini were the first to explore whether US laws that criminalised HIV non-disclosure had the impact that the lawmakers intended.
Zita Lazzarini: We found that whether you lived in a state with a law or without a law had absolutely no effect.
Scott Burris: Criminal law is generally a very blunt tool, anyway. And if you think about it, punishment and fear rarely brings out the best in people, when they’re making individual behaviour decisions. And certainly, when it comes to sex, criminal law has a very limited record of getting people to change their behaviour.
Carol Galletly has added much to the body of evidence on the impact of laws that criminalise HIV non-disclosure. Working with a number of colleagues, she published a number of studies, including this one in 2006 and this one in 2012 examining whether or not these laws are having the impact they were intended to have.
Carol Galletly: We thought of every single way these laws could possibly be effective. Do HIV-positive individuals reduce number of sex partners? Do they choose only positive sex partners more than people who don’t know about the law? Are they abstinent more? Do they practice safer sex more? Do they engage in oral sex or less risky activities? So we looked at all these things and the data just stacked up – there were no significant differences. The strongest predictor of disclosure was actually comfort with disclosure. So what I concluded was, if you really want people to disclose, then what you should probably do is increase their comfort, do interventions, do whatever. And don’t do laws that could jeopardize people disclosing.
Most laws and prosecutions focus on disclosure – in other words, whether or not the person with diagnosed HIV told their sexual partner before having sex. Whilst this may be the right thing to do, does this actually benefit HIV prevention? Eric Mykhalovskiy organised an international meeting on HIV prevention and criminal law in Toronto in April 2013 precisely because his own research found that criminalising HIV non-disclosure was having the opposite effect of what was intended.
Eric Mykhalovskiy: We see how significant now disclosure, or questions around disclosure, are within HIV prevention counselling, to the point that there is too much of a focus. You know, Barry Adam and others have emphasised repeatedly that disclosure is not an effective HIV prevention mechanism. And yet what seems to have happened is that the criminalisation of HIV non-disclosure has placed disclosure at the centre of people’s concerns around HIV prevention. And that is, I think, a serious challenge for people who are enlisted with the responsibility of trying to ensure that HIV transmission is lessened.
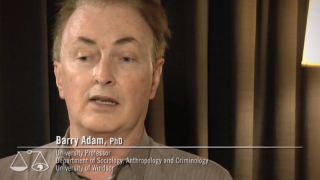
Barry Adam is Senior Scientist and Director of Prevention Research at the Ontario HIV Treatment Network and lead author of How criminalization is affecting people living with HIV in Ontario.
Barry Adam: Disclosure has become a bit of a red herring I think, in terms of HIV prevention because HIV prevention can and has for a long time happened without disclosure, anyways. To require disclosure doesn’t necessarily help. Sometimes, it could even hinder the process by creating a false sense of security among those who think that, if disclosure doesn’t happen, that their partner is negative. The social science evidence shows that, when people often get into the disclosure area, it’s in order to give themselves permission to have unprotected sex! People actually do have to know what their HIV status is in order to disclose it. And, there is a good deal of science these days that suggests that, it’s people who don’t know, who are newly infected, who are actually doing a lot of the infection.
Studies by Eric Mykhalovskiy, Chris Sanders and Martin French (the latter two are currently undertaking research studies and have not yet published their findings) have uncovered an unanticipated negative impact of HIV criminalisation on the healthcare workers who test and treat people with HIV, complicating their practice as public health professionals. They found that the criminal law is creating a chill, closing down discussions about HIV on both sides. (An in-depth report on the impact of HIV criminalisation on nursing practice can be found here.)
Chris Sanders: Criminalisation has complicated post-test counseling. Nurses are finding that clients shut down, they become very unwilling to speak openly about their sexual behaviour and they don’t want to share contact information because they’re worried that it might come back if they’re later charged with non-disclosure. And so, it makes nurses’ work more difficult. And that can impact HIV prevention as public health relies on contact tracing to be able to do quite a bit of their prevention work.
Martin French: I’m looking at this in Canada and the United States, and in spite of the fact that there are different approaches to public health I’m seeing some similar effects in terms of the anxiety that a number of providers are feeling about the issue of criminalisation as they counsel patients with respect to disclosure.
Trevor Hoppe found another, more sinister impact on healthcare workers. During his PhD research he discovered that some heath officials in Michigan’s public health system appeared to be invested in prosecuting people with HIV for not disclosing their status, resulting in some potentially problematic outcomes for HIV prevention.
Trevor Hoppe: This is the first piece of evidence that some health departments may be playing a role in facilitating criminal prosecutions. I can understand why people living in some of these communities would think twice before talking to health officials about their lives openly and honestly, given what health officials reported to me.
One of the most worrying aspects of HIV criminalisation is the additional disincentive it plays in a person’s willingness to take an HIV test: a significant number of new infections come from people who are undiagnosed. But testing is not just about knowing one’s HIV status to modify behaviour, it’s also the gateway to accessing HIV treatment and care.
New guidelines from the World Health Organization now highlight that HIV treatment works not only to keep people alive and well for a lifetime, but also prevents new infections by reducing HIV to undetectable levels. Where there is no virus, there can be no transmission. Since treatment is also prevention, then not testing or accessing treatment, hurts not only the individual but also the communities in which they live, harming the broader public health.
Laurel Sprague is the Research Director of the Sero Project, and oversaw their 2012 national HIV criminalisation survey.
Laurel Sprague: We asked people whether they thought it was not reasonable, somewhat reasonable or very reasonable to avoid getting an HIV test, or to avoid accessing treatment if someone tested positive because of HIV criminalisation. Those numbers should be zero. We shouldn’t have legal reasons for people not to get tested. We shouldn’t have a legal reason for people not to access care. And half of our respondents said that it was reasonable to avoid HIV testing because of HIV criminalisation and 42% of our respondents said it was reasonable, somewhat, or very reasonable to avoid getting HIV care once you’ve tested positive.
Patrick O’ Byrne is lead author of the 2013 review article, HIV criminal prosecutions and public health: an examination of the empirical research. He has also studied the impact of HIV prosecutions on gay men and documented how fear of HIV criminalisation has impacted their sexual and testing practices.
Patrick O’Byrne: Nobody – guys who were negative, guys who were positive – could make a distinction between the public health department and the police. It was a single institution. And this is problematic, right? How can you provide health care services when people think that you are a police agency? How do you provide care when people won’t access it? The laws have effectively rendered your HIV prevention health professionals useless.
Richard Elliott is the Executive Director of the Canadian HIV/AIDS Legal Network, and was an intervenor when the Supreme Court of Canada heard HIV criminalisation cases in 1998 and 2012.
Richard Elliott: How can it not have an impact on people and their decision as to whether or not to find out their HIV status, if you risk becoming a criminal. It may not at the end of the day dissuade a large number of people, but I think, it does dissuade a significant number of people and it probably, based on the evidence we have, dissuades some of those who are most likely to actually benefit from learning their HIV status, and all of the potential benefits to them, and others that may flow from that. So, why would we want to create an additional barrier, and why would we want to create a barrier to people actually seeking help from the helping professions? Because if we conscript those helping professions, to basically, become agents of law enforcement, that undermines their ability to help people, and that actually undermines the health of all of us.
Criminalisation is a divisive issue with strong opinions often informed by morality and a desire to achieve justice by punishing perceived wrongdoing. However, understanding the impact of HIV criminalisation on public health is critical to making informed policy decisions.
The 2013 UNAIDS guidance note, Ending overly-broad criminalisation of HIV non-disclosure, exposure and transmission: Critical scientific, medical and legal considerations aims to ensure that any application of criminal law in the context of HIV achieves justice and does not jeopardise public health objectives.
The guidance can be downloaded here.
More HARM Than GOOD [Trailer] (HJN, 2013)
Feature: Why overly broad HIV criminalisation is doing more harm than good
In many countries around the world, people with HIV are being made criminally liable for HIV prevention.
Despite strong recommendations against this overly broad use of the criminal law by UNAIDS and the Global Commission on HIV and the Law, the latest report from the Global Network of People Living with HIV and the HIV Justice Network highlights that new laws continue to be proposed and enacted, and more prosecutions are taking place than ever before.
The most commonly cited rationale of the criminal law is to deter morally unacceptable behaviour through fear of punishment. Scott Burris and Zita Lazzarini were the first to explore whether US laws that criminalised HIV non-disclosure had the impact that the lawmakers intended.
Zita Lazzarini: We found that whether you lived in a state with a law or without a law had absolutely no effect.
Scott Burris: Criminal law is generally a very blunt tool, anyway. And if you think about it, punishment and fear rarely brings out the best in people, when they’re making individual behaviour decisions. And certainly, when it comes to sex, criminal law has a very limited record of getting people to change their behaviour.
Carol Galletly has added much to the body of evidence on the impact of laws that criminalise HIV non-disclosure. Working with a number of colleagues, she published a number of studies, including this one in 2006 and this one in 2012 examining whether or not these laws are having the impact they were intended to have.
Carol Galletly: We thought of every single way these laws could possibly be effective. Do HIV-positive individuals reduce number of sex partners? Do they choose only positive sex partners more than people who don’t know about the law? Are they abstinent more? Do they practice safer sex more? Do they engage in oral sex or less risky activities? So we looked at all these things and the data just stacked up – there were no significant differences. The strongest predictor of disclosure was actually comfort with disclosure. So what I concluded was, if you really want people to disclose, then what you should probably do is increase their comfort, do interventions, do whatever. And don’t do laws that could jeopardize people disclosing.
Most laws and prosecutions focus on disclosure – in other words, whether or not the person with diagnosed HIV told their sexual partner before having sex. Whilst this may be the right thing to do, does this actually benefit HIV prevention? Eric Mykhalovskiy organised the workshop precisely because his own research found that criminalising non-disclosure was having the opposite effect of what was intended.
Eric Mykhalovskiy: We see how significant now disclosure, or questions around disclosure, are within HIV prevention counselling, to the point that there is too much of a focus. You know, Barry Adam and others have emphasised repeatedly that disclosure is not an effective HIV prevention mechanism. And yet what seems to have happened is that the criminalisation of HIV non-disclosure has placed disclosure at the centre of people’s concerns around HIV prevention. And that is, I think, a serious challenge for people who are enlisted with the responsibility of trying to ensure that HIV transmission is lessened.
Barry Adam is Senior Scientist and Director of Prevention Research at the Ontario HIV Treatment Network and lead author of How criminalization is affecting people living with HIV in Ontario.
Barry Adam: Disclosure has become a bit of a red herring I think, in terms of HIV prevention because HIV prevention can and has for a long time happened without disclosure, anyways. To require disclosure doesn’t necessarily help. Sometimes, it could even hinder the process by creating a false sense of security among those who think that, if disclosure doesn’t happen, that their partner is negative. The social science evidence shows that, when people often get into the disclosure area, it’s in order to give themselves permission to have unprotected sex! People actually do have to know what their HIV status is in order to disclose it. And, there is a good deal of science these days that suggests that, it’s people who don’t know, who are newly infected, who are actually doing a lot of the infection.
Studies by Eric Mykhalovskiy, Chris Sanders and Martin French (the latter two are currently undertaking research studies and have not yet published their findings) have uncovered an unanticipated negative impact of HIV criminalisation on the healthcare workers who test and treat people with HIV, complicating their practice as public health professionals. They found that the criminal law is creating a chill, closing down discussions about HIV on both sides. (An in-depth report on the impact of HIV criminalisation on nursing practice can be found here.)
Chris Sanders: Criminalisation has complicated post-test counseling. Nurses are finding that clients shut down, they become very unwilling to speak openly about their sexual behaviour and they don’t want to share contact information because they’re worried that it might come back if they’re later charged with non-disclosure. And so, it makes nurses’ work more difficult. And that can impact HIV prevention as public health relies on contact tracing to be able to do quite a bit of their prevention work.
Martin French: I’m looking at this in Canada and the United States, and in spite of the fact that there are different approaches to public health I’m seeing some similar effects in terms of the anxiety that a number of providers are feeling about the issue of criminalisation as they counsel patients with respect to disclosure.
Trevor Hoppe found another, more sinister impact on healthcare workers. During his PhD research he discovered that some heath officials in Michigan’s public health system appeared to be invested in prosecuting people with HIV for not disclosing their status, resulting in some potentially problematic outcomes for HIV prevention.
Trevor Hoppe: This is the first piece of evidence that some health departments may be playing a role in facilitating criminal prosecutions. I can understand why people living in some of these communities would think twice before talking to health officials about their lives openly and honestly, given what health officials reported to me.
One of the most worrying aspects of HIV criminalisation is the additional disincentive it plays in a person’s willingness to take an HIV test: a significant number of new infections come from people who are undiagnosed. But testing is not just about knowing one’s HIV status to modify behaviour, it’s also the gateway to accessing HIV treatment and care.
New guidelines from the World Health Organization now highlight that HIV treatment works not only to keep people alive and well for a lifetime, but also prevents new infections by reducing HIV to undetectable levels. Where there is no virus, there can be no transmission. Since treatment is also prevention, then not testing or accessing treatment, hurts not only the individual but also the communities in which they live, harming the broader public health.
Laurel Sprague is the Research Director of the Sero Project, and oversaw their 2012 national HIV criminalisation survey.
Laurel Sprague: We asked people whether they thought it was not reasonable, somewhat reasonable or very reasonable to avoid getting an HIV test, or to avoid accessing treatment if someone tested positive because of HIV criminalisation. Those numbers should be zero. We shouldn’t have legal reasons for people not to get tested. We shouldn’t have a legal reason for people not to access care. And half of our respondents said that it was reasonable to avoid HIV testing because of HIV criminalisation and 42% of our respondents said it was reasonable, somewhat, or very reasonable to avoid getting HIV care once you’ve tested positive.
Patrick O’ Byrne is lead author of the 2013 review article, HIV criminal prosecutions and public health: an examination of the empirical research. He has also studied the impact of HIV prosecutions on gay men and documented how fear of HIV criminalisation has impacted their sexual and testing practices.
Patrick O’Byrne: Nobody – guys who were negative, guys who were positive – could make a distinction between the public health department and the police. It was a single institution. And this is problematic, right? How can you provide health care services when people think that you are a police agency? How do you provide care when people won’t access it? The laws have effectively rendered your HIV prevention health professionals useless.
Richard Elliott is the Executive Director of the Canadian HIV/AIDS Legal Network, and was an intervenor when the Supreme Court of Canada heard HIV criminalisation cases in 1998 and 2012.
Richard Elliott: How can it not have an impact on people and their decision as to whether or not to find out their HIV status, if you risk becoming a criminal. It may not at the end of the day dissuade a large number of people, but I think, it does dissuade a significant number of people and it probably, based on the evidence we have, dissuades some of those who are most likely to actually benefit from learning their HIV status, and all of the potential benefits to them, and others that may flow from that. So, why would we want to create an additional barrier, and why would we want to create a barrier to people actually seeking help from the helping professions? Because if we conscript those helping professions, to basically, become agents of law enforcement, that undermines their ability to help people, and that actually undermines the health of all of us.
Criminalisation is a divisive issue with strong opinions often informed by morality and a desire to achieve justice by punishing perceived wrongdoing. However, understanding the impact of HIV criminalisation on public health is critical to making informed policy decisions.
The 2013 UNAIDS guidance note, Ending overly-broad criminalisation of HIV non-disclosure, exposure and transmission: Critical scientific, medical and legal considerations aims to ensure that any application of criminal law in the context of HIV achieves justice and does not jeopardise public health objectives.
The guidance can be downloaded here.
The HIV Justice Network has produced an accompanying video, ‘More HARM Than GOOD’ that we hope will be useful for both education and advocacy. Watch and/or download the video on our Vimeo channel: www.vimeo.com/hivjustice/moreharm