Translated from via Deepl.com. For the article in French and the Original article in Russian, please scroll down.
In Tajikistan, women living with HIV are denied help by their families. Many of them live in very precarious conditions, have no medical support and cannot find work.
HIV-positive women are one of the most discriminated against groups in Tajikistan. They are shunned by society as a whole, including their immediate families. Excluded, they can no longer work or have access to appropriate medical assistance. And yet, most of the time, these women pose no risk to the health of those around them.
To mark the “16 Days of Activism against Gender Violence” event and the International Day against HIV (Human Immunodeficiency Virus), Asia-Plus takes a look at the discrimination faced by these women.
A number of laws and documents exist in Tajikistan to directly or indirectly prevent discrimination against people living with HIV, as set out in an article by the NGO Foreign Policy Centre. In 2023, this list was supplemented by a new law on equality and the elimination of all forms of discrimination. According to human rights activists, it introduces the concept of “indirect discrimination”, which vulnerable groups often face. However, HIV-positive women are not entirely reassured by this new legal reference, as they already face direct discrimination on a daily basis.
Discrimination extending from the family to the medical community
“Despite the fact that HIV is not transmitted in everyday life and that antiretroviral (ARV) treatment (a treatment that slows down the development of the virus and the disease, editor’s note) reduces the viral load to a minimum, HIV-positive women are discriminated against at every street corner. And above all within their families”, explains Tahmina Khaïdarova, Tajikistan spokesperson for the Eurasian Women’s AIDS Network.
“As soon as her diagnosis is known, her family restricts contact with her and avoids her. This attitude then follows her wherever her situation becomes known.
Also read about Novastan: HIV positive and unemployed
Strange as it may seem, HIV-positive women often report discrimination from healthcare workers. These include dentists, surgeons, midwives and gynaecologists. Some doctors refuse to help women with HIV, and they have to find friendlier doctors through acquaintances.
“Yet modern medicine has eliminated all risk. Today, HIV is a chronic disease like diabetes. With the right ARV treatment and medical follow-up, HIV-positive women can become mothers of healthy children, but even some health workers don’t have this information,” explains Tahmina Khaïdarova.
Discrimination trivialised in the media
Local journalists also discriminate against women with HIV. The content devoted to this subject often takes a pejorative angle. The media confirm stereotypes, stigmatisation and prejudice, without explaining to the public what HIV is today.
“Even today, local journalists still use phrases like ‘AIDS: the plague of the 21st century’, ‘the terror of HIV‘ and other statements that have nothing to do with reality”, says Tahmina Khaïdarova.
Journalists often use intimidating language to talk about criminal cases (article 125 of the Tajik penal code, editor’s note) brought against women with HIV who are accused of knowingly infecting their husbands.
Discrimination, a source of violence against women
The Convention on the Elimination of All Forms of Discrimination against Women, to which Tajikistan has been a signatory for 30 years, states that gender inequality and discrimination are the primary reasons for violence against women.
In fact, any serodiscordant couple (where one partner is HIV-positive and the other is not, editor’s note) can fall foul of the first part of article 125 of the Tajik criminal code. This states: “knowingly placing another person at risk of HIV contamination”. It therefore refers not to factual contamination, but to the risk of infection. And all HIV-positive people who have a sexual partner are de facto exposing them to the risk of infection.
“But in reality, things don’t work like that. If a person is on ARV treatment, their viral load is reduced and even if they have unprotected sex, their partner will not catch HIV”, explains Tahmina Khaïdarova.
Women with HIV more discriminated against than men
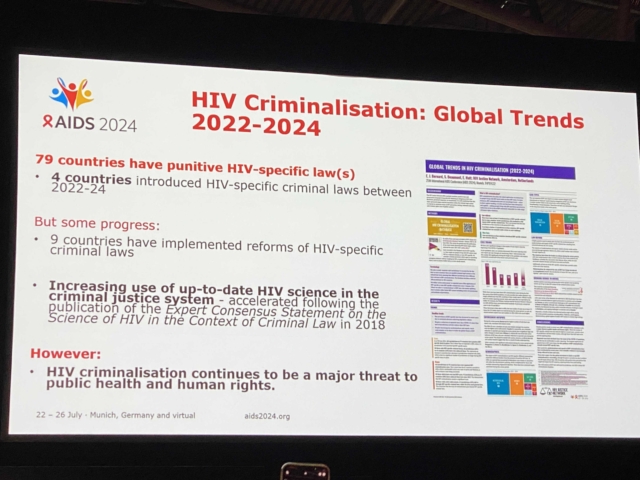
The spokeswoman tells us that at the twelfth International Conference on HIV Research, held in Brisbane from 23 to 26 July, the World Health Organisation presented new scientific and methodological recommendations relating to HIV. Among them is the indication of the viral load thresholds required for HIV infection.
This means that HIV-positive people who achieve a viral load level below this threshold by adhering to ARV treatment will not transmit HIV to their sexual partners. They have only a low risk of transmitting the virus vertically to their children.
“Many of the criminal cases that have resounded in Tajikistan have been launched on the basis of the first part of Article 125. But in reality, none of the ‘victims’ have been infected with HIV”, reveals Tahmina Khaïdarova. According to her, although men with HIV are also discriminated against, women are discriminated against to a greater extent.
Legal difficulties
The fact is that society still considers that a woman with HIV has had many sexual partners. However, according to statistics, sex workers represent only 1.7% of HIV-positive women in Tajikistan in 2022. All the others are women leading ordinary lives, sometimes housewives, who contracted the virus from their husbands.
“Not long ago, we were contacted by an HIV-positive woman. She was married, had a child, and her husband beat her. He even beat her during her pregnancy, so that she lost her second child”, says Tahmina Khaïdarova. “Although it was her husband who gave her HIV, her family blamed her.
“She left with her child, rented a room and found a job. But her ex-husband has got the child back and is threatening to deprive her of her rights over him because she is HIV-positive, uneducated and on a modest salary on which she can’t look after her child.”
The courts also discriminate against women, even those without HIV. That’s why there’s no guarantee that if her husband does try to deprive her of her child, the judge will see the absurdity and injustice of the situation.
Translated from the Russian by Paulinon Vanackère and edited by Coraline Grondin
Contaminer son épouse puis l’accuser : ces femmes tadjikes séropositives face aux discriminations sociales
Au Tadjikistan, les femmes atteintes du VIH se voient refuser l’aide de leur famille. En grande précarité, beaucoup ne bénéficient pas d’accompagnement médical et ne trouvent pas de travail.
Tadjikistan
Les femmes séropositives sont un des groupes les plus discriminés au Tadjikistan. La société entière se détourne d’elles, y compris leur famille proche. Exclues, elles ne peuvent plus travailler ni avoir accès à une aide médicale adaptée. Pourtant, la plupart du temps, ces femmes ne représentent aucun risque pour la santé de leur entourage.
A l’occasion de l’événement « 16 jours d’action contre les violences de genre » et de la journée internationale de lutte contre le VIH (virus de l’immunodéficience humaine), Asia-Plus se penche sur les discriminations que ces femmes rencontrent.
Diverses lois et documents existent au Tadjikistan pour empêcher directement ou indirectement la discrimination des personnes atteintes du VIH, rassemblées dans un article de l’ONG Foreign Policy Centre. En 2023, cette liste a été complétée d’une nouvelle loi sur l’égalité et l’élimination de toutes les formes de discrimination. Selon les défenseurs des droits humains, elle fait apparaître le concept de « discriminations indirectes » auxquelles les groupes vulnérables sont souvent confrontés. Cependant, les femmes séropositives ne sont pas pleinement rassurées par cette nouvelle mention légale car elles font déjà face à des discriminations directes au quotidien.
Des discriminations s’étendant de la famille à la communauté médicale
« Malgré le fait que le VIH ne se transmet pas dans la vie quotidienne et que le traitement antirétroviral (ARV) (un traitement qui ralentit le développement du virus et la maladie, ndlr) atténue au minimum la charge virale, les femmes séropositives sont discriminées à chaque coin de rue. Et avant tout dans leur famille », explique Tahmina Khaïdarova, porte-parole pour le Tadjikistan du Réseau des femmes eurasiennes sur le SIDA.
« A peine son diagnostic est-il connu que sa famille restreint ses contacts avec elle et l’évite. Puis, cette attitude la suivra partout où sa situation est connue. »
Aussi étrange que cela puisse paraître, les femmes séropositives rapportent souvent des discriminations de la part des travailleurs de la santé. Parmi eux, dentistes, chirurgiens, sages-femmes ou gynécologues. Des médecins refusent de porter assistance aux femmes atteintes du VIH et elles doivent trouver des docteurs plus amicaux en passant par des connaissances.
« Pourtant, la médecine moderne a fait disparaître tout risque. Aujourd’hui, le VIH est une maladie chronique comme le diabète. Avec un traitement ARV adéquat et un suivi médical, les femmes séropositives deviennent mères d’enfants en bonne santé, mais même certains travailleurs de la santé n’ont pas ces informations », explique Tahmina Khaïdarova.
Les discriminations banalisées dans les médias
Les journalistes locaux discriminent également les femmes atteintes du VIH. Les contenus consacrés à ce thème prennent souvent un angle péjoratif. Les médias confirment des stéréotypes, des stigmatisations et des préjugés, sans expliquer au public ce que représente aujourd’hui le VIH.
« Encore aujourd’hui, on rencontre chez les journalistes locaux des formulations comme « le sida : la peste du XXIème siècle », « la terreur du VIH » et autres affirmations qui n’ont rien à voir avec la réalité », raconte Tahmina Khaïdarova.
Souvent, les journalistes utilisent des formules intimidantes pour parler de cas d’affaires pénales (article 125 du code pénal tadjik, ndlr) ouvertes contres des femmes atteintes du VIH et accusées d’avoir consciemment contaminé leur mari.
Les discriminations, sources de violences faites aux femmes
La Convention sur l’élimination de toutes les formes de discrimination à l’égard des femmes, dont le Tadjikistan est signataire depuis 30 ans, affirme que l’inégalité et la discrimination de genre sont les raisons premières des violences faites aux femmes.
En fait, tout couple sérodiscordant (dont un des partenaires est séropositif et l’autre non, ndlr) peut tomber sous le coup de la première partie de l’article 125 du code pénal tadjik. Celle-ci indique : « placer consciemment une autre personne en position de risque de contamination au VIH. » Ainsi, elle fait référence non pas à la contamination factuelle, mais au risque d’infection. Et tous les séropositifs qui ont un partenaire sexuel le placent de fait face au risque d’être contaminé.
« Mais en réalité, les choses ne fonctionnent pas ainsi. Si une personne est sous traitement ARV, la charge virale est diminuée et même en cas de relation sexuelle non protégée, son partenaire n’attrapera pas le VIH », explique Tahmina Khaïdarova.
Les femmes atteintes de VIH plus discriminées que les hommes
La porte-parole raconte qu’à la douzième conférence internationale pour la recherche contre le VIH, qui a eu lieu du 23 au 26 juillet dernier à Brisbane, l’Organisation mondiale de la santé a présenté de nouvelles recommandations scientifiques et méthodiques en relation avec le VIH. Parmi elles, l’indication des seuils de charge virale nécessaires à la contamination par le VIH.
Ainsi, les personnes séropositives qui atteignent un niveau de charge virale inférieur à ce seuil grâce à l’observance du traitement ARV ne transmettent pas le VIH à leurs partenaires sexuels. Elles n’ont qu’un risque faible de transmettre verticalement le virus à leurs enfants.
De nombreuses affaires pénales qui ont résonné au Tadjikistan ont été lancées en s’appuyant sur la première partie de l’article 125. Mais en réalité, aucune des « victimes » n’a été contaminée par le VIH », révèle Tahmina Khaïdarova. Selon elle, bien que les hommes atteints de VIH soient aussi soumis à la discrimination, les femmes le sont davantage.
Des difficultés face à la justice
Le fait est que la société considère toujours qu’une femme atteinte du VIH a eu beaucoup de partenaires sexuels. Cependant, selon les statistiques, les travailleuses du sexe représentent seulement 1,7 % des femmes séropositives au Tadjikistan en 2022. Toutes les autres sont des femmes menant une vie ordinaire, parfois femmes au foyer, qui ont contracté le virus par leur mari.
« Il y a peu, nous avons été contactées par une femme séropositive. Elle était mariée, a eu un enfant, et son mari la battait. Il l’a battue même pendant sa grossesse, si bien qu’elle a perdu son deuxième enfant », raconte Tahmina Khaïdarova. « Bien que ce soit son mari qui lui a donné le VIH, sa famille l’a accusée, elle. »
« Elle est partie avec son enfant, loue une chambre et a trouvé un travail. Mais son ex-mari a récupéré l’enfant et la menace de la priver de ses droits sur lui parce qu’elle est séropositive, sans éducation et avec un salaire modeste avec lequel elle ne peut pas s’occuper de son enfant. »
Les tribunaux aussi discriminent les femmes, mêmes non atteintes du VIH. C’est pourquoi rien ne garantit que si son mari tente effectivement de la priver de son enfant, le juge s’aperçoive de l’absurdité et de l’injustice de la situation.
La rédaction d’Asia-Plus
Traduit du russe par Paulinon Vanackère
Сам заразил, но жену обвинил. Женщины с ВИЧ подвергаются в Таджикистане дискриминации
Женщинам с диагнозом ВИЧ в Таджикистане отказывают в поддержке не только родственники, но помощь могут не оказать даже врачи.
Женщины с ВИЧ – одна из самых дискриминируемых групп в Таджикистане. От них отворачивается всё общество, включая самых близких родственников; они не могут найти работу или получить медицинское обслуживание. При этом чаще всего никаких рисков здоровью окружающих эти женщины не несут.
В честь международной акции «16 дней активных действий против гендерного насилия» и Всемирного дня борьбы против СПИДа «Азия-Плюс» рассказывает о дискриминации, с которой они сталкиваются.
В Таджикистане существует целый список самых разных законов и документов, которые прямо или косвенно защищают людей, живущих с ВИЧ от дискриминации.
В прошлом году этот список пополнился еще одним законом «О равенстве и ликвидации всех форм дискриминации». В нем, к удовлетворению правозащитников, появилось понятие «косвенной дискриминации», с которой чаще всего сталкиваются уязвимые группы в Таджикистане. Однако женщин, живущих с ВИЧ, это важное описание в законе, не успокаивает, потому что именно эта группа населения каждый день сталкивается с прямой дискриминацией.
«Несмотря на то, что ВИЧ не передается бытовым путем, а современная АВР-терапия (терапия, которая замедляет развитие вируса и заболевание, – ред.) до минимума снижает вирусную нагрузку, дискриминации женщина с ВИЧ подвергается на каждом шагу, – говорит Тахмина Хайдарова, руководительница Сети женщин, живущих с ВИЧ. – Прежде всего, внутри семьи.
Как только выясняется, что у нее положительный статус, родственники сокращают с ней контакты, избегают ее. Со временем такое отношение будет сопровождать ее везде, где узнают о ее статусе».
Как это ни странно, отмечает Тахмина, женщины, живущие с ВИЧ, часто жалуются на проявление дискриминации со стороны медицинских работников: стоматологов, хирургов, акушеров, гинекологов. Доктора отказываются оказывать помощь женщинам с ВИЧ и им приходится искать дружественных специалистов через знакомых.
«При этом современная медицина сняла все риски: ВИЧ сегодня это такое же хроническое заболевание, как сахарный диабет. При адекватной АВР-терапии и врачебном уходе, женщины с ВИЧ становятся матерями здоровых детей, но даже у медицинских работников нет актуальной информации на этот счет, – поясняет Тахмина Хайдарова.
Дискриминируют женщин с ВИЧ и местные журналисты. В контенте, посвященном женщинам с ВИЧ, часто присутствуют уничижительные обороты, медиа транслируют стереотипы, стигму и предрассудки, и не объясняют аудитории о том, что собой сегодня представляет ВИЧ.
«До сих пор в материалах местных журналистов встречаются такие обороты, как “ВИЧ/СПИД – чума 21 века”, “ВИЧ-террор” и прочие утверждения, не имеющие ничего общего с реальностью», – говорит Хайдарова.
Часто журналисты используют устрашающие обороты при освещении случаев возбуждения уголовных статей (125 ст. УК РТ, – ред.) в отношении женщин с ВИЧ, которые якобы осознанно заражают мужчин.
В Конвенции о ликвидации всех форм дискриминации в отношении женщин (КЛДЖ), подписанной Таджикистаном 30 лет тому назад, говорится, что гендерное неравенство и дискриминация являются первопричинами насилия в отношении женщин.
«По сути, под первую часть 125 статьи УК Таджикистана могут попасть и все дискордантные пары (в которых один партнер с положительным статусом ВИЧ, другой – с отрицательным, – ред.). В этой части прописано: “Заведомое поставление другого лица в опасность заражения ВИЧ‐инфекцией”, то есть это не фактическое заражение, а риск заражения. И все люди с положительным ВИЧ-статусом, у которых есть половой партнер, фактически, ставят его под угрозу риска заражения.
Но по факту это не так: если человек принимает АРВ-терапию, его вирусная нагрузка снижена, и даже в случае незащищенного секса, его партнер не заразится ВИЧ», – говорит руководительница Сети женщин, живущих с ВИЧ.
Женщинам с ВИЧ достается больше
Она рассказывает, что на двенадцатой международной конференции по научным исследованиям ВИЧ, которая проходила 23–26 июля в австралийском городе Брисбен, Всемирная организация здравоохранения представила новые научные и методические рекомендации в отношении ВИЧ.
В них были приведены ключевые пороговые значения вирусной нагрузки при ВИЧ.
Так, ВИЧ-положительные лица, у которых благодаря соблюдению режима антиретровирусной терапии достигнут неопределяемый уровень вирусной нагрузки, не передают ВИЧ своим сексуальным партнерам и подвергаются низкому риску «вертикальной» передачи вируса своим детям.
«Многие громкие уголовные дела в Таджикистане были возбуждены именно по первой части статьи 125 УК. Но на деле никто из “пострадавших” не заразился ВИЧ», – объясняет Тахмина Хайдарова.
По ее словам, несмотря на то, что мужчины с положительным статусом ВИЧ также подвергаются дискриминации, женщинам достается больше.
Дело в том, что до сих пор общество считает, что женщина с ВИЧ – это женщина, у которой было много сексуальных партнеров. Тогда как по статистике секс-работниц среди женщин с ВИЧ в Таджикистане на конец 2022 года всего 1,7 %. Все остальные – это, как правило, обычные женщины-домохозяйки, которые заразились от своих мужей.
«К нам недавно обратилась женщина, живущая с ВИЧ: она была замужем, родила ребенка, муж ее ужасно избивал. Избивал даже во время беременности так, что она потеряла второго ребенка, – рассказывает Тахмина. – Несмотря на то, что именно муж заразил ее ВИЧ, его семья во всем обвиняла саму женщину.
Она ушла от него с ребенком, сняла комнату, устроилась на работу. Но бывший муж забрал ребенка и теперь угрожает лишить ее родительских прав, потому что у нее положительный статус ВИЧ, нет образования и маленькая зарплата, на которую она не может содержать ребенка».
Учитывая тот факт, что таджикские женщины даже без ВИЧ подвергаются дискриминации в судебных органах, нет никакой гарантии, что в случае, если мужчина, о котором рассказывает Тахмина, действительно попытается лишить свою бывшую жену родительских прав, в суде увидят всю абсурдность и несправедливость ситуации.
Подробнее: https://asiaplustj.info/ru/news/tajikistan/society/20231201/sam-zarazil-no-zhenu-obvinil-zhentshini-s-vich-podvergayutsya-v-tadzhikistane-diskriminatsii