GAC holds policy dialogue on human rights, HIV and law Ghana needs a roadmap for the proposal of an HIV/AIDS prevention and control law to consolidate gains made so far by the Ghana Aids Commission (GAC) and its partners.
Uganda: As second reading of controversial national HIV law awaits, activists hope regional HIV law – with no HIV criminal statute – will take precedence
Activists in Uganda are seeing an opportunity to shoot down the country’s controversial HIV Bill that criminalises transmission of the Aids virus and enforces mandatory testing, after President Yoweri Museveni signed a more liberal one proposed by the East African Community. They want Uganda’s parliament to incorporate into law the EAC HIV and Aids Prevention Bill (EAC HIV Bill) that President Museveni signed last week. More than 30 NGOs in Uganda find the national law that is awaiting a second reading in parliament offensive, saying that it could exacerbate the spread of HIV. Laws passed by the East African Legislative Assembly take precedence over national laws. President Museveni can also prevail upon the Ugandan parliament to drop the bill.
As Kenya and Uganda assent to East African Community's Regional AIDS Law, the lack of an HIV criminalisation statute apparently holds back Tanzania and Burundi
Having a common regional approach to the HIV and Aids pandemic is an important step for the East African Community, as the five member states get ready for closer integration. The increased trade and labour migration that comes with closer economic ties will invariably create situations where large numbers of foreign nationals travel or relocate freely in their territories.
Nigeria: Advocates successfully argue for removal of HIV criminalisation clause from draft HIV and AIDS Anti-Discrimination Act
Advocates in Nigeria have successfullly argued to remove a clause criminalising the ‘willful or deliberate spead of HIV’ from the latest draft of the long-awaited HIV and AIDS Anti-Discrimination Act.
Last week, the National Agency for the Control of AIDS (NACA) held a two-day stakeholders forum on the much delayed national anti-discrimination law. The meeting aimed to re-energize the passing of the bill into law, and to ensure that it incorporated international human rights conventions and standards as they relate to people living with HIV.
The national law also aims to harmonise state anti-discrimination laws. Currently, three states – Lagos, Enugu and Cross River State – include HIV criminalisation statutes in their their laws.
The vaguely-worded proposed HIV criminalisation statute of the draft national anti-discrimination bill read as follows:
Section 31 Willfull or Deliberate Spread of HIV Virus
Any person, having known his/her seropositive status, deliberately transmits the HIV directly or indirectly shall be guilty of an offence and, upon conviction be sentenced up to twelve months imprisonment or fine of up to N500,000 or both.
At the meeting, many stakeholders proposed to keep the HIV criminalisation statute in the bill, but civil society organisations, led by the Network of People Living with HIV and AIDS in Nigeria (NEPWHAN), successfully advocated against the statute.
Instead, the provisions of the anti-discrimination bill were expanded from covering workplace discrimination to be broadly applicable at the workplace, school, correctional institutions, religious institutions, and in society at large.
The draft harmonized bill as proposed with input from NEPWHAN and other civil society organisations is below. Note the absence of Section 31. Although this is unlikely to be the final wording of the law, it certaily shows how successful advocacy can remove problematic provisions in otherwise supportive and enabling HIV-related laws.
Draft Harmonized Nigerian HIV and AIDS Anti-Discriminational Act 2013
UK: Updated guidance on HIV transmission, the law and the work of the clinical team now published
The British HIV Association (BHIVA) and the British Association for Sexual Health and HIV (BASHH) have produced updated guidance on HIV Transmission, the Law and the Work of the Clinical Team.
This guidance is aimed at those working in the field of HIV medicine, especially clinicians, but will also be of use to general practitioners and people living with HIV who want to understand the legal and medical basis for some of their care decisions.
The guidance begins with a clear statement against HIV criminalisation:
BHIVA and BASHH believe that this use of the law is unhelpful and potentially harmful to public health and support UNAIDS recommendations to limit the use of criminal law and the Oslo declaration view that a “non-punitive, non-criminal HIV prevention approach” is preferable.
Covering the law in England & Wales as well as Scotland, the document aims to provide information and guidance on managing issues related to sexual transmission of HIV based on current scientific evidence. It applies generic ethical and professional principles but with a greater emphasis on providing a confidential environment in which extremely sensitive matters can be frankly and fully discussed. This enables appropriate care of people with HIV and benefits public health by encouraging individuals to access testing and treatment. Within this framework this document sets out the roles and responsibilities of health care professionals when caring for individuals living with HIV.
Consistent with the recent BHIVA and the Expert Advisory Group on AIDS (EAGA) position statement on the use of antiretroviral therapy to reduce HIV transmission, the guidance notes:
In most situations the appropriate use of antiretroviral treatment is at least as effective as condoms in preventing sexual transmission of HIV. This is accepted by the [Crown Prosecution Service of England and Wales] and [Scottish Crown Office and Procurator Fiscal Service] so it is likely that evidence showing that the defendant was taking effective antiretroviral treatment at the time of the alleged transmission may be used to demonstrate that they were not reckless.
The guidance also clearly states that healthcare professionals “must be mindful of their duty not to work beyond their expertise in legal matters. For people with HIV, advice must include the routes of HIV transmission and how to prevent transmission, with information about safer sexual practices, the use of condoms and suppression of viral load. Advice must be given in a non-judgmental way.”
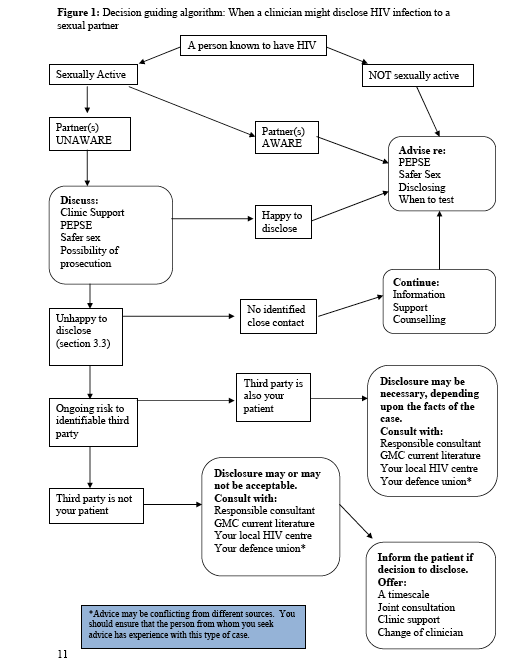
It also discusses issues of confidentiality, noting that “it is important when considering breaching confidentiality to weigh up all potential harms as there may be situations where disclosure of HIV status to protect a sexual partner results in considerable harm to an individual e.g. domestic violence. In situations where a health care professional believes that an HIV positive individual continues to put sexual contacts at risk their duties and subsequent action depend upon the type of contact.” See Figure 1 below.
The guidance also clearly states that “no information should be released to the police unless patient consent has been verified or there is a court order in place, except in very limited circumstances defined by the [General Medical Council].”
Importantly, it also notes that only individuals can make complainants to the police “and health care workers should remain impartial during discussions with patients.”
Finally, it provides clear advice to both help prevent transmission of HIV to sexual partners and to avoid prosecution for ‘reckless’ HIV transmission. Accordingly, people with HIV should do at least one of the following:
- Use a male or female condom fitted correctly along with water-based lubricant. Individuals doing this are unlikely to be seen as reckless for legal purposes. In the event of a condom split, it is advisable to disclose HIV status in order to support the partner’s decision whether or not to obtain post-exposure prophylaxis (PEPSE), which should be taken within 72 hours. The need for PEPSE will depend upon the type of sexual activity and the HIV viral load. An assessment of the risk should be undertaken by a clinician according to the BASHH PEPSE guidelines. Disclosure in these situations would suggest that the person with HIV was not reckless.
- Adhere to effective (suppressed viral load) antiretroviral medication. There is growing evidence of extremely low/minimal risk of transmission when plasma HIV is fully suppressed with the use of antiretroviral medication. In some situations an undetectable viral load can afford protection equivalent to or greater than that of condoms. A person with HIV is unlikely to be seen as reckless when relying on a suppressed viral load instead of condom use if they have been counselled accordingly by an HIV clinician or similar medical authority. It is recommended that this discussion is documented in the patient’s medical records.
In addition people with HIV should be advised that disclosure of HIV positive status to a partner before sex is important to support informed agreement around risk and safer sex behaviours. To avoid successful prosecution an individual who is not taking effective antiretroviral medication and does not use a condom must disclose their HIV status to sexual partners before sex takes place.
The entire guidance is reproduced below.
Norway: National Association of People Living with HIV responds to Norwegian Law Commission report
Yesterday was the deadline for written responses to the Norwegian Law Commission report which shocked and disappointed HIV and human rights advocates in Norway and around the world on its release last October.
After spending almost two years examining every aspect of the use of the criminal law to punish and regulate people with communicable diseases (with a specific focus on HIV) the Commission recommended that Norway continues to essentially criminalise all unprotected sex by people living with HIV regardless of the actual risk of HIV exposure and regardless of whether or not there was intent to harm. The only defence written into the new draft law is for the HIV-negative partner to give full and informed consent to unprotected sex that is witnessed by a healthcare professional.
Since then, Professor Matthew Weait has published Some Reflections on Norway’s Law Commission Report on Criminal Law and the Transmission of Disease on his blog highlighting some of problems with the arguments used in the report.
We have also published an interview with Kim Fangen, the only member of the Commission to vote against the use of a specific law to control and punish people with HIV and other sexually transmitted infections, which presented an alternative vision.
Today, we publish the English translation of the written response by Nye Pluss, the Norwegian national association of people living with HIV.
The organisation found that, overall, the report has three key weaknesses:
• It does not take into account the formidable global challenges related to HIV and AIDS and is not consistent with the international responsibilities that Norway has to follow-up recommendations that have come from a variety of organisations, including UNAIDS.
• It does not take into account the medical advances that have taken place in the HIV field over the past few years., in particular that HIV treatment is, in fact, now prevention, and that testing and treatment (“treatment as prevention”) is one of the most important preventive measures to combat the global HIV epidemic.
• It does not acknowledge that HIV criminalisation will help to prevent effective contact tracing and counselling, and thus influence the HIV response in the wrong direction. A desire for the use of punishment is, therefore, at the expense of public health.
Nye Pluss recommends that the Government and Parliament reject the choice of the majority’s conclusions in this area and remove the particular provisions of the Criminal Code.
The HIV Justice Network fully supports their arguments and conclusions and hopes that Norways parliamentarians follow the lead of Labour’s Håkon Haugli and The Conservative Party’s Bent Høie who came out against any specific law last July.
Below is the English translation of the Nye Pluss response, shortened and paraphrased in some areas, but with their full agreement and permission. The original Norwegian version can be read here.
Nye Pluss’s board has read and discussed the Norwegian report. Our perspective is that, as people living with HIV, all aspects of Norwegian HIV policies, including any special penal provision, must have the net result of fewer new infections. Our primary perspective is therefore one of public health.
We have found that, overall, this report has three key weaknesses:
• It does not take into account the formidable global challenges related to HIV and AIDS and is not consistent with the international responsibilities that Norway has to follow-up recommendations that have come from a variety of organisations, including UNAIDS.
• It does not take into account the medical advances that have taken place in the HIV field over the past few years., in particular that HIV treatment is, in fact, now prevention, and that testing and treatment (“treatment as prevention”) is one of the most important preventive measures to combat the global HIV epidemic.
• It does not acknowledge that HIV criminalisation will help to prevent effective contact tracing and counselling, and thus influence the HIV response in the wrong direction. A desire for the use of punishment is, therefore, at the expense of public health.
Below, we elaborate our views on these three objections.
Norway’s international responsibility in the fight against HIV
The fight against HIV and AIDS is one of the biggest challenges we face in the world: two million die every year due to AIDS-related illnesses. Around 35 million people live with HIV globally. Nearly three million are newly infected with HIV each year. Norwegian authorities have a responsibility to contribute to the international HIV response. We therefore believe that the discussion on penalising HIV exposure or transmission in Norway must be seen in relation to the international challenges we face. This report does not live up to those challenges.
At page 184 the report states:
“UNAIDS ‘work is global, but is mainly aimed at countries where the prevalence of HIV and AIDS is high. UNAIDS has no European office, such as WHO and recommendations etc. have a global objectives and are hardly suitable for Scandinavian or European conditions. The committee’s review will be largely based on our cultural context, which can be very different from the global.”
It therefore concludes that UNAIDS’ work and recommendations specifically relating to criminal laws are not relevant for Norway, while Norwegian authorities support UNAIDS efforts globally. This is, in our opinion, a somewhat arrogant and culturally discriminatory attitude to the situation in other countries. Although Norwegian law is only applicable in Norway, we expect that Norwegian laws at home should also follow, and are not contrary to, the beliefs and policies that we export to other countries in the world.
“Treatment as prevention” – a medical breakthrough in the fight against HIV
A medical breakthrough took place when the first effective HIV medicines appeared in 1996. In countries where there was good access to these medicines, the number of AIDS-related deaths fell quickly and drastically. Treatment as prevention is, perhaps, just as big a breakthrough – we now know that effective HIV medication prevents new HIV infections. New research shows that the risk of infection is reduced by 96%, more than any other prevention method.
[Several paragraphs discuss international policy relating to ‘treatment as prevention’….]
Nye Pluss notes with surprise that the report only once refers to “treatment as prevention” and even then in a way that gives the impression that the authors of this section have not acquired up-to-date knowledge of the issue. It is regrettable that such an important resource which claims to provide a basis for Parliament to examine Norwegian HIV policy in a holistic context – not least relating to the criminal law – treats such an important part of international HIV policy so superficially. We believe that it is a serious academic failure not to discuss the effects of punitive sanctions on earlier testing and treatment.
Criminal law regulation of serious infectious diseases – an obstacle in the fight against HIV
HIV criminalisation has been a growing problem in many countries around the world in recent years. Criminalisation helps to maintain stigma and prevent openness about HIV, and is thus an unwanted obstacle in HIV treatment and prevention. In addition, HIV criminalisation in many countries works to suppress women and minority groups that are particularly vulnerable to HIV.
Nye Pluss believes that the criminalisation of HIV exposure and transmission has been a barrier to effective HIV prevention in Norway. In some groups, annual HIV figures have tripled over the last ten years, compared with the previous decade.
A future, efficient Norwegian HIV policy will depend on effective and efficient testing, counselling, contact tracing and treatment, such as a “treatment as prevention” strategy. Effective testing of affected populations, effective tracing of possible infected sexual partners and effective treatment is, along with condoms and awareness, cornerstones of reducing new infections in Norway.
For those of us living with HIV, it is important that a future Norwegian strategy is successful, so that fewer people acquire HIV in Norway….One such major obstacle to achieve reduced infection figures is the criminalisation of HIV through a special provision in the Criminal Code, as advocated by the majority of the committee behind the report.
In the pharmaceutical industry….the manufacturer must show that the drug’s harmful effects do not exceed its positive effects… Surely it is possible that an HIV law will negatively impact vulnerable groups of people with HIV who have immigrated from countries with non-democratic regimes, who are more likely to go underground if there are threats of punitive sanctions, so that testing, disclosure, contact tracing, treatment and counselling is not available to them? Nye Pluss consider it obvious that there exists such a legitimate doubt and that this is precisely one of the reasons that some MPs have requested a separate investigation of the criminal law as it relates to HIV. “It is therefore surprising that the majority of the commission’s members argue, without any scientific evidence, that there would be no negative impact to an HIV law.”
Moreover, many members of the committee suggest that “decriminalization could be perceived as a signal that infecting others or exposing others to infection, is no longer a serious matter”(page 248). This is an unscientific, tautological statement based on the completely undocumented assumption that because HIV exposure and transmission is criminalised in Norway it has worked as a prevention tool, and that decriminalising it would lead to more infections, despite a lack of any evidence supporting this.
Nye Pluss believes the committee majority here are completely wrong, and we can refer to international research studies that support this.
[A summary of studies from Canada (O’Byrne, 2012), the US (Sero, 2012), Scotland (Bird and Leigh-Brown, 2001), and England (Whitlock, Warwick et al, 2010) showing a negative impact of HIV criminalisation follows.]
Nye Pluss finds it surprising that the majority of the Committee does not seem to be familiar with the research that has been done in recent years which shows that HIV criminalisation has unique negative impacts on willingness to test, to disclose to sexual partners, and in the creation of uncertainty amongst health care workers and counsellors. This somewhat surprising rejection of the existence of such research and thus a lack of discussion of such readily available research, weakens, in Nye Pluss’s perception, a range of the majority’s conclusions on the importance of the criminal law’s impact on public health: not to discuss the importance of documented research in this area is a serious mistake and results in the majority’s conclusions on public health failing in crucial ways.
Another key point of the debate around a penalty provision for people with HIV is the growth we have seen in HIV figures among particularly vulnerable groups, such as men who have sex with men, over the last ten years…The extremely serious issue that is raised is whether the relatively large number of prosecutions over the past decade has affected HIV testing behaviour, thus increasing the number of untreated individuals, resulting in more new infections.
It is a serious public health issue when there is a tripling of HIV infection among men who have sex with men for the last ten years in Norway. We are in absolutely no doubt that public health has not benefitted from the use of the Penal Code, and are of the opinion that the studies and analyses conducted to date, and as mentioned above, show with great clarity that the increased number of criminal trials over the last decade have impacted Norwegian society and public health in an extremely negative way. Nye Pluss cannot see that the Criminal Code’s provisions against HIV, which the majority recommend, will result in fewer HIV cases.
Nye Pluss believes that the latest scientific advances pertaining to HIV treatment and prevention will do perfectly well by themselves without assistance from the criminal law, including those few cases where restrictive measures for infection control law would be needed against an individual.
Conclusions
Nye Pluss believes that the Committee’s recommendations to maintain the criminal regulation of HIV exposure and transmission and other general dangerous diseases, would undermine Norway’s international responsibility to participate in a common front to combat HIV in the world.
We must recognise that since 100% safe sex is not possible it would be impractical to allow the courts to put a specific limit on what is punishable in a world where sex is a universal activity for the continuation of humanity … To punish a select few who have not mastered ‘safer sex’ – defined narrowly as condom use – is neither a fair or an effective tool in this fight, but rather the opposite.
No matter where you draw the line regarding what is, or is not, a criminal offense, a specific penal code criminalising HIV exposure and transmission will prevent effective prevention, early testing, contact tracing, treatment and counselling, and will put a spoke in the wheels of the “treatment as prevention” strategy that promises to be the breakthrough in the fight against HIV. That the criminal law should be both an obstacle to international responsibility and to effective measures for domestic public health in this area is unacceptable for society.
Nye Pluss recommends that the Government and Parliament reject the choice of the majority’s conclusions in this area and remove the particular provisions of the Criminal Code.
Philippines updates HIV law to provide supportive and enabling legal environment
A MEASURE seeking to strengthen the country’s comprehensive policy on the Human Immunodeficiency Virus and Acquired Immune Deficiency Syndrome (HIV-AIDS) is expected to be approved on third and final reading when Congress resumes session next week. One of the proponents of House Bill 6751, Ilocos Norte Rep.
Lawyers petition government for protection to mark Human Rights Day | SW Radio Africa
The Zimbabwe Lawyers for Human Rights (ZLHR) marched from Harare Gardens through the streets of the capital on Thursday, to commemorate International Human Rights Day, which falls on December 10th. The lawyers delivered petitions to the Supreme Court, the High Court, Parliament, the Ministry of Justice and Legal Affairs and the Attorney General’s Office, asking for protection for legal practitioners while they do their work. Makoni said the lawyers expect the level of intimidation and harassment of lawyers to increase as the country heads towards elections, because that is when violence levels go up and lawyers are called upon to represent victims and perpetrators.
Fiji lawmakers move to decriminalise sex work
allAfrica.com: Kenya: Its Criminal to Sterilise a HIV Postive Woman Without Consent
Any doctor found guilty of sterilizing a HIV positive woman without her consent,is liable to prosecution. Public Health Minister Beth Mugo says sterilization of HIV Positive Women violates their human rights as guaranteed in the constitution.