HIV: Prosecution or Prevention? HIV Is Not a Crime
A chapter from the book The War on Sex edited by David M. Halperin and Trevor Hoppe.
Iowan Nick Rhoades is HIV-positive and has had an undetectable viral load for many years, making it virtually impossible for him to sexually transmit the virus. When he had sex with a man he met online in 2008, he also used a condom. Despite these protective measures, Rhoades was prosecuted and convicted for not disclosing his HIV status to his partner before they had sex. He was sentenced to 25 years in prison and lifetime sex offender registration.
Willy Campbell is serving 35 years in Texas for spitting at a police officer; David Plunkett served over six years in a New York state prison before an appeals court ruled that saliva could not be considered a “deadly weapon” in New York State. Monique Howell Moree was charged by the U.S. Army for failing to disclosure her HIV-positive status to a partner in South Carolina before having sex with him, even though the partner said he didn’t want her charged and that she told him to use a condom. Kerry Thomas is serving 30 years in Idaho, even though his accuser agrees that he always used a condom.
All over the United States — and in much of the world — people living with HIV/AIDS (PLHIV) are facing criminal penalties for nondisclosure of their HIV status prior to having sex or for perceived or possible exposure to, or transmission of, HIV. About two-thirds of U.S. states have HIV-specific criminal statutes, laws that only apply to PLHIV.
Most people believe the law should apply equally to all and that creating different statutes for different parts of society based on immutable characteristics — whether it is gender, sexual orientation, race, physical ability, or genetic makeup — is a bad idea. Yet here we are doing exactly that, creating a viral underclass in the law with one group singled out for different treatment.
Sero Project, a network of PLHIV combating HIV criminalization, has documented more than 1,300 instances of charges led under HIV-specific statutes. But HIV criminalization isn’t constrained by geography; in every state, regardless of whether there is an HIV-specific statute, PLHIV can and often do face more serious charges or harsher sentencing under regular criminal statutes than do HIV-negative individuals accused of the same crimes. Texas and New York do not have HIV-specific statutes, but as mentioned, have incarcerated PLHIV because they considered their saliva dangerous.
These statutes and prosecutions create an illusion of safety for those who do not have HIV or do not know their HIV status, putting the entire burden of HIV prevention on those who have been tested and know they have HIV. The statutes undercut the fundamental public health message that HIV prevention is a shared responsibility and that everyone should act in such a way as to maintain their own health and protect themselves from contracting HIV or other sexually transmitted infections.
Decades-long sentencing and required sex offender registration are not unusual punishments for HIV-related crimes in the United States, even though actual HIV transmission is seldom (less than 5 percent of cases) a factor in these prosecutions. Many cases boil down to whether the PLHIV can prove they disclosed their status to their partners in advance of intimate physical contact; it doesn’t matter whether there was even a risk of HIV transmission. People living with HIV charged under prostitution or assault statutes frequently face significantly more severe penalties solely because they have HIV. They sometimes face charges for spitting, scratching, or biting that are “pile-on” charges, driven by accusations made by law enforcement, first responders, or prison guards.
The first HIV criminalization laws in the United States were passed in the late 1980s and early ’90s, largely in response to a provision of the Ryan White Care Act that required states, in order to qualify for funding, to demonstrate an ability to prosecute what was then labeled “intentional transmission.” At the time many considered any intimate contact with an HIV-positive person a life-threatening risk; contracting HIV was believed by many to be tantamount to a death sentence.
A second wave of statutes was enacted after the introduction of combination therapy in the mid-1990s, which fundamentally changed what an HIV-positive diagnosis meant. What was once thought a death sentence had become a chronic but manageable long-term health condition.
As it became understood that PLHIV were surviving much longer, the public’s perception of PLHIV also changed. Rather than objects of pity facing a “death sentence,” PLHIV became seen as viral vectors, potential infectors — an inherent threat to society. Living longer meant PLHIV would be around longer to infect others.
The criminal justice and public health systems began to define and treat PLHIV as a dangerous population, one that needed to be sought out, tracked down, tested, reported, listed, tagged, monitored, regulated, and, increasingly, criminalized.
While the statutes were used in the early years disproportionately often against heterosexual African American men (often in conjunction with other criminal charges), today they are used more broadly, typically in circumstances where there was no intent to harm, often when there was no other crime involved, and frequently for behaviors that pose no or little risk of HIV transmission.
Beyond the blatant injustice, HIV criminalization is also horrible public health policy, because it discourages people at risk from getting tested for HIV and makes those who do test positive less trustful of public health authorities.
To be liable for prosecution, one must get tested for HIV and know one’s HIV status. Current HIV criminalization punishes this responsible behavior — getting tested — and privileges the ignorance of not knowing one’s HIV status. Yet new cases of HIV are transmitted in disproportionate numbers by those who have not been tested and do not know they have it; those who do get tested and know they have HIV are far less likely to transmit HIV than those with HIV who do not know it.
Although the HIV-specific statutes were passed by state legislatures with the intent to reduce HIV transmission, the evidence increasingly shows that the statutes may be having the reverse effect.
The Sero Project’s 2012 survey of more than 2,000 PLHIV in the United States revealed that at least 25 percent of the respondents knew one or more individuals who were afraid to get tested for fear of facing criminalization. Research has shown that HIV criminalization makes those who do test positive for HIV less likely to cooperate with traditional disease prevention measures, like partner notification programs, or with treatment adherence programs. Most recently, a study found that HIV-negative gay men who knew they lived in a state with an HIV criminalization statute were more likely to engage in unprotected intercourse.
Repeal of HIV criminalization statutes is necessary both to protect the rights of people with HIV and to reduce the transmission of HIV.
An individual who demonstrates a premeditated malicious intent to harm another person can be prosecuted under existing assault statutes, whether they use a gun, a baseball bat, their fists, or a virus. The HIV-specific statutes are unnecessary and, worse yet, they stigmatize people with HIV/AIDS, discourage people at risk from accessing testing and treatment services, and feed a public bloodlust for punishment. In short, they are worsening the epidemic.
The prevention of HIV — or preventing any sexually transmitted infection — is a shared responsibility, but that does not mean there is not harm inflicted when someone misleads another person and transmits an infectious disease. In those circumstances, the injured party may seek recourse in the civil courts or possibly through a restorative justice process.
In any case, incarceration of PLHIV does not necessarily prevent further HIV transmission, as there is significant HIV transmission within penal environments, where condoms are seldom available.
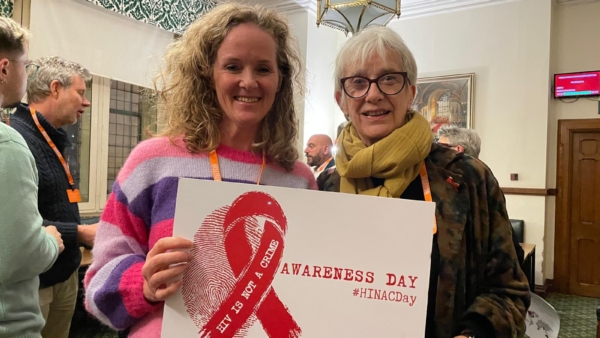
Advocacy to repeal HIV-specific statutes, modernize public health statutes concerning perceived or possible exposure to, or transmission of, HIV and other infectious diseases, and educate law enforcement, prosecutors, and other actors in the criminal justice system has been under way for several years.
A network of survivors of HIV criminalization prosecutions, launched in 2010, has helped to educate and mobilize affected communities. This HIV criminalization reform advocacy has received support from public health professionals and policy leaders, including the Presidential Advisory Council on HIV/AIDS, the National Alliance of State and Territorial AIDS Directors, UNAIDS, and the American Medical Association.
The first national conference on HIV criminalization in the United States was held in June 2014 at Grinnell College in Grinnell, Iowa. Organized primarily by PLHIV — including participation by a dozen PLHIV who had been prosecuted for “HIV crimes” — the conference included participants from 28 states. It focused on how HIV criminalization affects communities of color, transgender women, sex workers, and gay men. It also showed the impact of HIV criminalization on how members of those communities (and others) access HIV prevention, testing, and treatment and whether they decide to disclose their HIV status. Finally, the conference highlighted effective strategies for reform.
The only state, so far, to modernize their statute substantively in recent years has been Iowa, where the conference was held. After a four-year education and lobbying effort led by Nick Rhoades and other PLHIV in the state, the Iowa legislature repealed its HIV-specific statute in 2014. The legislature replaced it with a new statute that addressed several infectious diseases, required a higher standard of intent to harm, and established tiered punishments. Similar efforts are under way in about a dozen states. A few weeks later, the Iowa Supreme Court overturned Rhoades’s conviction and removed the sex offender registration requirement for all others previously convicted under the Iowa statute.
HIV criminalization is an extreme manifestation of stigma. That is particularly true of HIV-specific statutes that create a viral underclass in the law, establishing a different criminal law for one segment of society based on an immutable characteristic. Despite the biomedical advances in the treatment of HIV, HIV-related stigma remains stubborn, driven in significant part by HIV criminalization.
It is time we learned a basic lesson: HIV can be prevented or it can be prosecuted, but not both.