Yesterday Professor Matthew Weait, Professor of Law and Policy at Birkbeck College, University of London delivered a stirring lecture to the public health professionals involved in implementing Norway’s HIV strategy. As Norway is currently reconsidering its criminal code as it relates to HIV and other infectious diseases, ‘Criminalisation and Effective HIV Response’ was a clear clarion call to “recognise that HIV is not a legal problem capable of a legal solution, but a public health issue to be dealt with as such.”
What I would urge you to recognise is that the appeals for change are being made not only by people living with HIV and the civil society organisations advocating on their behalf, but increasingly by health professionals, virologists, epidemiologists and others who have come to recognise that punitive responses to HIV are counter-productive and damaging in efforts to respond effectively to the spread of the virus. This is a critically important point, and their voice needs to be heard.
With Matthew’s permission, I am publishing the entire lecture below. You can also download the full text (with full detailed footnotes and references) from Matthew’s blog.
 |
| Courtesy of Charlotte Nördstrom |
As a country which many in the world look to for progressive policy-making grounded in evidence and human rights principles, Norway’s response to HIV is not simply a matter of national importance, but is of significance both to the developing countries to which it provides economic and other assistance in the fight against endemic HIV, and to high-income countries whose epidemics are similarly limited and concentrated in particular population groups.
Your current national strategy – Acceptance and Coping – states as follows:
The comprehensive aim of this strategy is that at the end of the strategy period, Norway will be a society that accepts and copes with HIV in a way that both limits new infection and gives persons living with HIV good conditions for social inclusion in all phases of their lives.
The strategy document sets out a number of specific goals, each of which discusses measures that will be taken in order to deliver on the strategy. My focus today is on the way criminalisation of HIV transmission and exposure might impact on that strategy. I will start, though, with some background and context.
1. International Thinking and National Law
At the 26th special session of the UN General Assembly in 2001, States party to the International Covenant on Economic, Social and Cultural rights (including Norway) declared their commitment to
… enact, strengthen or enforce, as appropriate, legislation, regulations and other measures to eliminate all forms of discrimination against and to ensure the full enjoyment of all human rights and fundamental freedoms by people living with HIV/AIDS and members of vulnerable groups …
This commitment is yet to be realised. Since the beginning of the epidemic new and existing legislative measures have been introduced and enforced that impede rather than further the central goal of reducing onward transmission of HIV, of minimising the spread of the epidemic, and protecting the rights of PLHIV and those most at risk of infection.
In a 2010 Report, the UN Special Rapporteur on the Right to Health referred to this commitment in the context of the criminalisation of HIV transmission and exposure. Drawing on the best available evidence he emphasised that criminalisation has not been shown to limit the spread of HIV, that it undermines public health efforts and has a disproportionate impact on vulnerable communities.
Drawing on the UNAIDS International Guidelines on HIV/AIDS and Human Rights and more recent UNAIDS/UNDP policy, he reiterated that the criminal law should only be deployed in very limited circumstances. In particular, people should not be prosecuted where there is no significant risk of transmission, where they are unaware of their HIV positive status, do not understand how HIV is transmitted, have disclosed their status (or honestly believe their partner to know it), failed to disclose because of a fear of violence or other serious negative consequences, took reasonable precautions against transmission, or have agreed on a level of mutually acceptable risk.
Norway, in common with most other countries, falls significantly short of the UNAIDS guidance and of the Special Rapporteur’s recommendations. Its current criminal law imposes liability irrespective of a person’s viral load, those who transmit HIV non-intentionally, and on those who merely expose others to the risk of infection. Also, and more exceptionally, it allows for the criminalisation and punishment of those who engage in unprotected sex, even when they have disclosed their HIV positive status to their partner and where the partner has consented to the risk of transmission. Although its penal code allows for the criminalisation of other serious diseases, almost all cases that have been brought to the courts have concerned HIV – and so although it is not an HIV-specific law in theory, the practice is very different.
2. The Enforcement of Law
This use of the criminal law has placed Norway – along with its Scandinavian and Nordic neighbours, at the top of the leader board of HIV criminalisation in Europe, and very high globally. When we look at rate of convictions per 1000 PLHIV in the European region, we see a higher rate of conviction in northern European countries, especially those in Nordic and Scandinavian countries.
This variation in intensity of criminalization as measured by convictions seems strange at first glance, especially when you contrast it with the HIV prevalence estimates.
It is especially notable that the bottom three countries with respect to criminalisation (Italy, France, UK) have – conversely – the highest numbers of people living with HIV, and (in general) higher than average prevalence.
What, then, might be explanations for this? We have to be cautious, given the non-systematic nature of the data collection; but I do think that we can begin to understand the pattern if we think about some of the social, cultural and historical differences between countries in the region.
So, for example, we can see that the top five criminalising countries in the region all have laws which impose liability for the reckless or negligent exposure (and thus have a wider potential scope for criminalisation). We can also see that these same countries all have high confidence in their judicial systems (which may go some way towards accounting for a person’s willingness to prosecute after a diagnosis, believing that their complaint will be dealt with efficiently and fairly). Even more interestingly, I think, are the correlations that we see when we look at variations in interpersonal trust, as measured by the World Values Survey.
Here we can see the top five countries in the region with respect to interpersonal trust (and the only countries where the majority of respondents trusted other people), are all in the top half of criminalizing countries, with rates of conviction in excess of 1 / 1000 PLHIV.
These correlations between interpersonal trust and conviction rates in the region become even more interesting when we learn that, according to reliable empirical research, the Scandinavian and Nordic countries have a lower fear of crime, are less punitive in their attitudes to those who commit crime, and – in general – have lower rates of imprisonment for convicted offenders than other countries. If this is the case, why would HIV transmission and exposure criminalization be so high?
My answer to this is tentative, but it seems plausible to suggest that the sexual HIV cases that get as far as court and a conviction are ones which are paradigm examples of breach of trust. It is not inconsistent for a society to have a lower than average generalised fear of crime, or lower than average punitive attitudes, and at the same time to respond punitively to specific experiences of harm, especially when that arises from a belief that the person behaving harmfully could have behaved otherwise and chose not to. Indeed, it seems entirely plausible that where there are high expectations of trust, breaches of trust (for example, non-disclosure of HIV status) are treated as more significant than where value in trust is low. Combine this with countries (such as your own and Sweden) which are committed to using law to ensure public health, and which consequently are prepared to using it to respond to the risk of harm (HIV exposure), as well as harm itself (HIV transmission), and we can see why the pattern of criminalization appears to be as it is.
3. Impact of Criminalisation on PLHIV and Most at Risk Populations
What is the impact of criminalisation?
This is a difficult question to answer, because it depends on what we mean by impact. First, there is the impact on the individual people who have been, and continue to be, prosecuted – people who have been investigated, convicted, jailed and publicly shamed, sometimes simply for having put others at risk, sometimes for transmitting HIV unintentionally, sometimes when they have been completely open about their status with a partner in a relationship which subsequently breaks down. For these people, being HIV positive and failing to live up to the exacting standards the law in this country, and others in this region, demands of them has turned them into criminals with all the social and economic disadvantages that entails. Here we could think specifically of your own fellow country man Louis, who had a charge of transmission dropped when it transpired that he was not the source of his partner’s infection, but is still being prosecuted for exposure.
Second, and critically, there is the impact on public attitudes towards, and responsibility as regards HIV, PLHIV and sexual health generally. Here I am not talking just about the individual experience of the two Thai women in Bergen who stopped in a bar for a drink after shopping and, in front of other customers, were thrown out by the owner because of a recent case in the town involving a Thai sex worker (from that point on, being Thai themselves (though legally in the country and married to Norwegian men) made them guilty, positive and dangerous simply by association). I am talking more of the broader impact that such an example illustrates.
Criminalisation, because it places responsibility for transmission risk on people with diagnosed HIV, serves to reinforce the idea that responsibility for one’s own sexual health belongs with those people. The existence of criminal law provides people who have consciously taken risks with an official mechanism for declaring their victim status. It provides grown, adult, men who have unprotected sex with migrant sex workers an opportunity to deny any responsibility they might have for actually taking responsibility themselves. It provides people (in Norway) who in fact consent to sex with a person who has disclosed his or her positive status the opportunity to take revenge if the relationship breaks down. If we can blame someone else for misfortune, or for being in situations where there is a risk of harm, it is only natural that some of us will; and the sensationalist media coverage (as bad here as it is anywhere in the world) merely serves to confirm this and to sustain the ignorance which the FAFO study highlighted. The headlines are, as you well know, always in the form “HIV-man (or woman) exposes x number of women (or men) to HIV.” They are never in the form “X number of people put themselves at risk by having unprotected sex”.
Finally, I would just like to mention Maria (not her real name) who I interviewed here in Oslo in March 2012. For her, a mother of two children who was contacted by the police about the arrest of a man she had had a sexual relationship with (but who was not in fact the source of her HIV infection) the trial in which she was made to be a complainant has resulted in her being so afraid of legal repercussions that she has not had sex for eighteen months. For Maria, and people like her, a guilty verdict does not necessarily result in closure, and it does not result in a reversal of sero-status. It simply creates another potential criminal who better beware. If, as Acceptance and Coping states, Norway is serious about reducing the number of new infections, enabling people to feel secure in testing and in discussing their positive status more openly, it must recognise that criminalisation of the kind that exists in this country does nothing to assist in those endeavours.
4. Barriers to Change
What, then, are the barriers to change? I ask this question recognising that the Commission led by Professor Aslak Syse has yet to report on its findings and make recommendations, and here I will mention only two.
The first thing I would say here is that here are many in the Scandinavian and Nordic region who are calling for a change in the law. However, there has been, and continues to be, among politicians and policy makers – as well as among some public health professionals – a scepticism about calls to decriminalise non-deliberate HIV transmission and exposure.
Take politicians first. Their scepticism stems, I think, from a belief that arguments in favour of decriminalisation when made by advocacy organisations are – in effect – arguments for being allowed to practise unsafe sex with impunity: without consequence. If a gay man living with HIV argues that he should not be punished if he has unprotected sex, or does not disclose his status to a partner, or happens to transmit HIV during consensual sex (even when this is the last thing he wishes to do) it is very easy to hear that as someone claiming a right to be irresponsible. Put simply, the fact that at a national level in this region the decriminalisation advocacy work has been pursued largely – though not entirely – by civil society organisations has resulted in a less than sympathetic response from those in a position to deliver change – especially those elected politicians whose principal concern is their immediate electorate and public opinion more generally. Nor, for a long time, has the medical profession been entirely supportive. For doctors, especially those in official public health positions at national and regional level, it has been problematic to support those who seem to wish to challenge their role in protecting the health of society generally. For health professionals, arguments for repealing the coercive powers given to them under communicable disease legislation, or of the criminal law that provides the final sanction against those who do not comply with regulations, are easily read as arguments for allowing people with HIV the right to undermine the very thing it is their responsibility to achieve: as a right to put healthy people at risk of disease and illness.
Faced with the way in which their arguments have been interpreted by those with political power, it is small wonder that those appealing for change have met with limited success, despite arguments consistent with those of expert international organisations (such as UNAIDS). What I would urge you to recognise is that the appeals for change are being made not only by people living with HIV and the civil society organisations advocating on their behalf, but increasingly by health professionals, virologists, epidemiologists and others who have come to recognise that punitive responses to HIV are counter-productive and damaging in efforts to respond effectively to the spread of the virus. This is a critically important point, and their voice needs to be heard.
The second factor that sustains the legitimacy of punitive laws in a country, and makes their reform difficult, is the nature of the epidemic in that country. Like other Nordic countries, Norway’s HIV epidemic is localised both socially and geographically. It is predominantly an urban disease affecting MSM and migrants from high-prevalence regions in Africa and Asia. Recognition of this has led to targeted prevention strategies, which is of course welcome; but it has also contributed to the ignorance about HIV among the general population (as shown by the FAFO study), and – critically, I think – to a perception that HIV is, and remains, someone else’s problem. Epidemiologically this may be correct. HIV does not, in general, impact directly on the lives of the vast majority of Norwegians. Few will know someone living with HIV, and even fewer someone who is open about his or her positive status. A consequence of this is that measures which would be seen as gross infringements of civil liberties and personal freedom if applied to the general population are seen as a reasonable and legitimate response. It is as if HIV were a snake that has found its way into a party full of animal rights activists. They cannot simply kill it (that would be wrong, and there are some limits to how one may reasonably respond to phobias) but it is justifiable to take any containment measures necessary to stop it getting any closer.
If you doubt this, consider the following two questions. First, we know that a significant number of new transmissions of HIV are from those who are newly infected and undiagnosed. If the criminal law on exposure and transmission were logical, should it not be applied to all those who have unprotected sex with a partner, who have had unprotected sex in the past, and who do not have a recent negative test result? And if we think non-disclosure is a justification for criminal liability, should we not criminalise all those who fail to disclose the fact that they have had unprotected sex in the past and are uncertain of their HIV status? Being HIV positive is not the relevant risk: infectiousness is.
Why don’t we do that when it is the logical approach? Because such rules would apply to the vast majority of adults in Norway, not merely to a containable and definable sub-section of those adults. And even those who might respond to this proposition by pointing out that undiagnosed HIV is far more common among MSM and migrants would have a hard time justifying criminalising all unprotected homosexual (but not heterosexual) sexual activity, and the unprotected sexual activity of migrant people from high-prevalence regions with native Norwegians. This would be seen, I suspect, as a grossly discriminatory and offensive approach – despite the fact that it makes far more sense than the one that you have here.
As to the second question, consider this. Norway, in common with its neighbours, has a strong tradition of overseas aid, and an official, publicised commitment to providing assistance to developing countries in their fight against HIV and AIDS. Indeed, the Government of Norway has publicly stated that it “ … wishes to focus on how legislation and public services can do more to reduce vulnerability and increase dignity and better cooperation into the fight against AIDS”.
The question therefore is: should Norway encourage the high-prevalence countries to which it provides support to adopt its legal model their HIV response? Put simply, do you think it would be appropriate to criminalise HIV transmission, exposure and non-disclosure where it is endemic? My guess is that your answer to that would be no. But if the answer is no, you must ask yourselves – as matter of fundamental ethics – why not? Why is it appropriate to respond punitively to PLHIV living in Norway when to do so in Botswana, or Malawi, or Swaziland would be wrong?
It seems to me that the answer to this question, even if it is a difficult and uncomfortable one to acknowledge, is that for as long as HIV only affects a small and definable minority punishment is defensible. As long it is “over there”, among the gays and the migrants and the IDUs, and for as long as coercive powers will not impact on the vast majority of the population, criminalisation is something that can be legitimated and politically defended without fear of popular protest. If this is correct, it is particularly offensive and pernicious. Exposure is exposure wherever it takes place in the world; transmission is transmission; HIV is HIV; disclosure is either to be required as a matter of principle, or not. If criminalisation is not something that one country would countenance for human beings in countries in which HIV continues to be a real and immanent threat, and – critically – human beings for whom HIV infection is far less easy to manage, and still results in significant mortality, then on what possible principled basis is it justifiable to use the criminal law against those in one’s own country, where HIV is a manageable condition and where the quality of life for diagnosed PLHIV is as high as it possibly could be? If there is any substance to the claim that the legal response to PLHIV in Norway is discriminatory – which many of its critics suggest – that substance finds its expression here.
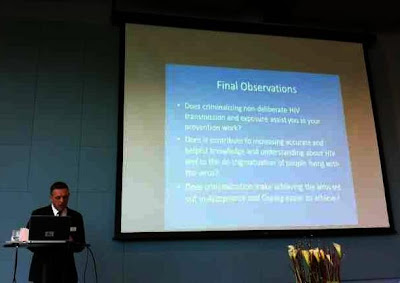
5. Final Observations
Norway is placed better than any other nation at the present moment to reform its law so that it complies with UNAIDS recommendations. The work of the Law Commission, which will report in the autumn of 2012, has been more focused and comprehensive than any other initiative I know of. Its report will, I have no doubt, present arguments both for and against the present law, and those arguments will be supported by the best available evidence. Ultimately, though, legal reform is in the hands of politicians, and their concerns extend beyond the logic of prevention. What those politicians need is the support of those who work in the field, at the sharp end of HIV prevention, diagnosis and treatment. Without that, it will be all too easy to adopt minimal reforms that do not go to the heart of the matter, or to kick the report into the long grass and carry on as before. It is not for me to tell you what your law should be. All I can do is urge you to read the Oslo Declaration, published here just recently, and to watch the video accompanying that. All I can do is encourage you to recognise that the authors of the HIV Manifesto, a radical initiative demanding the repeal of paragraph 155 of the Penal Code, was not written by people who simply want to have sex without consequences but by intelligent, rational and thoughtful people. All I can ask you to do is to recognise that HIV is not a legal problem capable of a legal solution, but a public health issue to be dealt with as such. All I can suggest is that in thinking about this complex topic you ask yourself the following simple questions.
Does criminalising non-deliberate HIV transmission and exposure assist you in your prevention work?
Does it contribute to increasing accurate and helpful knowledge and understanding about HIV and to the de-stigmatisation of people living with the virus?
And does criminalisation make achieving the aims set out in Acceptance and Coping easier to achieve?
If the answer to any or all of these questions is no, then the arguments for HIV criminalisation of the kind and intensity that currently exist in this country are not, I would suggest, as strong as those against.



